PTSD and Traumatic Brain Injury: What’s the link?
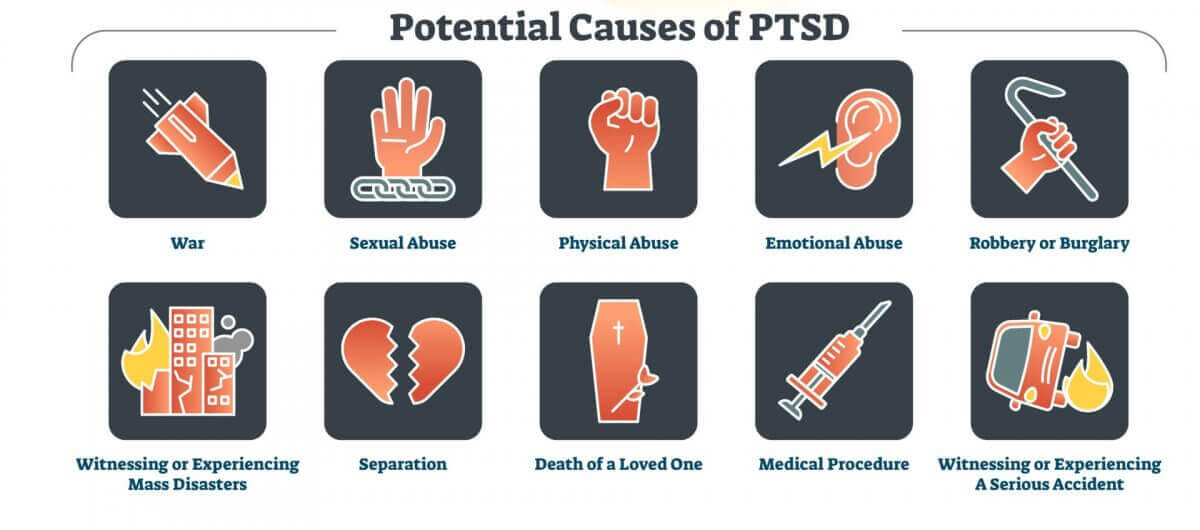
War veterans probably spring to mind when most people think of post traumatic stress disorder (PTSD). But many kinds of traumatic events can cause people to develop PTSD.
About 60-75% of Americans will experience at least one traumatic event during their lifetime, and the majority will experience more than one. Events could include natural disasters, life-threatening accidents, physical or sexual assault, the sudden death of a loved one, or the diagnosis of a serious illness; even simply witnessing such events can be traumatic.
Not everyone who goes through a traumatic event will develop PTSD. Most people will process the trauma and move on. However, twenty percent will develop PTSD.
PTSD may take months or even years to develop. It can potentially affect your physical, mental, emotional, and cognitive health in a number of ways, including:
- Intrusive symptoms such as memories, flashbacks, or nightmares
- Avoidance of people, places, etc. that trigger memories of the event
- Negative changes in thinking patterns and mood
- Emotional changes, including heightened emotions or conversely feeling numb
- Heightened arousal and reactivity
- Cognitive impairments such as memory, attention, or concentration struggles
- Sleeping problems and insomnia
The full list of symptoms can be found here.
PTSD can develop after physical trauma, such as an accident or natural disaster, or due to psychological trauma alone, such as seeing someone die or being mugged at gunpoint.
PTSD and Traumatic Brain Injury
PTSD shares a considerable amount of overlap with traumatic brain injury (TBI), and researchers are trying to figure out why. Not only are the two conditions difficult for clinicians to distinguish between, but they also frequently occur together.
A large study of US Army soldiers who fought in Operation Iraqi Freedom reported that 43.9% of the soldiers who had TBI with loss of consciousness also met diagnostic criteria for PTSD. Another study reported that having a TBI doubled the chance of developing PTSD.
Traumatic brain injuries are generally caused by a blow to the head, injuries that pierce the skull and brain, or things such as whiplash that can cause the brain to bump into the skull. Like PTSD, TBI is not limited to combat vets; every year, at least 1.5 million people in the US experience a TBI.
Depending on the severity, TBI can be mild, moderate, or severe. It’s even possible to have a TBI and not even know it! Mild TBIs (mTBI), also known as concussion, can involve the following symptoms.
- Headache
- Dizziness
- Nausea
- Fatigue or drowsiness
- Speech problems
- Sensory issues such as a bad taste in the mouth
- Sensitivity to light or sound
For moderate TBIs, the symptoms above can be more severe and also accompanied by the loss of consciousness.
Most people with mild and even moderate TBI recover within days to months. However, about 15% will show symptoms of post-concussive syndrome a year later. The symptoms include most of the same ones that could have immediately followed the trauma. But it could also include persistent emotional challenges such as mood lability, anxiety and/or depression, and cognitive impairments like mental slowness or memory or concentration issues, like brain fog.
Interestingly, those who have a mild TBI are more likely to develop PTSD than those with more severe brain injuries. The likely reason is that those who experience a more violent blow to the head tend to have amnesia around the traumatic event, ironically sparing them from the flashbacks, nightmares, bad memories, and more that are often caused by PTSD.
What’s the connection?

The same traumatic event can cause TBI, PTSD, or both, especially if the traumatic event involved psychological as well as physical trauma, such as war combat or domestic violence.
One condition can also affect the course of the other. For example, PTSD that develops following a car accident could complicate recovery from brain injuries sustained; conversely, a TBI may block the person’s ability to get emotional closure from the psychological aspects of the event.
How do they cause cognitive issues?
Until recently, researchers didn’t understand exactly what these conditions were doing in the brain, and in particular how they affected cognition.
According to this review, TBI and PTSD represent “brain disorders with disruptions in neural networks that communicate via long axonal pathways through white matter tracts, termed the “connectome.” The connectome is the brain’s “wiring” pattern; the sum total of billions of neurons and the pathways or routes that they use to carry out their function.
Both TBI and PTSD have shown to produce neural inflammation, excitotoxicity, and oxidative stress within the brain. These processes, all of which can affect one another, represent normal functions in the body that, under every day conditions, don’t cause harm. If these functions get pressed into service too often or for too long though, they can kick into overdrive and quickly spiral out of control, leading to cellular damage and physical changes in the brain.
For example, the amygdala is largely responsible for the “raw data” of emotions that arise in the body. But it’s your prefrontal cortex that actually works with the amygdala to regulate emotions. Studies have shown that a critical connection between the prefrontal cortex and amygdala may be broken in brains with TBI or PTSD, which could explain the commonly seen lack of emotional control.
The bottom line
PTSD and TBI can both be debilitating conditions that greatly affect everyday life for those who suffer from them. However, recent research into the neural mechanisms of these disorders has opened the door for the discovery of new treatment options.
Could I have a Traumatic Brain Injury and Not Know It?
As the years go by, many of us chalk up lapses in memory as a side effect of aging. But if you’re also experiencing headaches, trouble concentrating, and thinking clearly, then something more serious may be to blame: a traumatic brain injury. What, a brain injury? Surprisingly, yes. Brain injuries are more common than most people realize, and left unchecked they can wreak serious havoc in your life. Fortunately, the latest scientific advancements, such as hyperbaric oxygen treatment protocol, show promise in helping treat traumatic brain injuries.
According to the Brain Injury Association, more than 2.8 million people sustain a traumatic brain injury (TBI) every year, and TBI-related deaths are highest among older adults. Since symptoms of a traumatic brain injury can sometimes take years to manifest, many people don’t even realize that they have one until problems show up later in life. That’s right: the fall you had in the 1990s could actually be the cause of your headaches and brain fog today.
TBIs can cause all sorts of cognitive problems and can even lead to permanent disabilities if left unchecked. You don’t even need to directly hit your head to obtain one, either. But the good news is that with proper detection, traumatic brain injuries can be treated, including at centers such as Aviv Clinics. That’s why we’ve put together this helpful guide with everything you need to know about TBIs and how to determine if you may have one.
What is a Traumatic Brain Injury?
A traumatic brain injury (TBI) is exactly what it sounds like. It’s a form of brain injury that occurs when an external trauma is inflicted upon the brain. This trauma can impair your brain’s ability to communicate with the rest of your body, and the effects can differ depending on the part of your brain that was injured. Damage can range from mild to severe and there is not always a loss of consciousness.
The most common form of a mild TBI is a concussion, which is caused by a violent shaking or rattling of the brain. Common causes for TBIs include: Sports injuries, Falling off a bike or horse, Military injuries, Being assaulted or struck, Being in a car accident, Falling and hitting your head.
Any kind of scenario involving your brain hitting your skull can cause a TBI, such as whiplash from a car accident. Although the potential for sustaining damage is greater if you were knocked unconscious, you don’t have to lose consciousness to experience negative effects. Even mild brain injuries can cause symptoms to appear in the long term.
TBI symptoms checklist
What are the symptoms of a traumatic brain injury? Just like the severity of a TBI can vary, so too can the severity of the symptoms you experience.
Signs of a concussion or mild TBI include:
– Headaches and dizziness
– Nausea and vomiting
– Changes in sleep patterns
– Confusion or Memory Loss
– Fatigue or lethargy
– Difficulty concentrating
– Difficulty making decisions
– Mood changes like depression or irritability
Although many people feel the effects immediately after sustaining a brain injury, symptoms can show up at any time, even years later. This delay means that many people never make the connection between hitting their head and cognitive problems experienced later in life.
In some cases, a TBI may never be properly diagnosed because the person who sustained it never lost consciousness or never went to the doctor afterward. Many people suffer needlessly because they never realize they sustained a TBI to begin with, and the effects of an untreated TBI can be devastating.
TBIs can even lead to more sensory problems like blurred vision, ringing in the ears (tinnitus), or even difficulty understanding language and communicating properly (aphasia). And because TBIs and dementia can have similar symptoms, it’s important to know what you’re dealing with so that you can receive the proper treatment.
How do you detect a TBI?
There are different ways to evaluate for a TBI. Brain injuries can cause two distinct types of damage: structural and metabolic. Structural damage is caused by physical damage to the brain, such as bleeding. Metabolic damage affects the brain cells themselves. A CAT scan or MRI is the first step to detecting obvious structural damage in the brain. But there can be more subtle damage to your brain that these scans might miss, especially if your injury is years old. This is where more advanced techniques come into play.
Functional MRIs or SPECT scans can detect metabolic damage in the brain tissue.
These scans can reveal improperly functioning brain cells even years after the bleeding has stopped.
From there, your healthcare provider can move forward with treatment options.
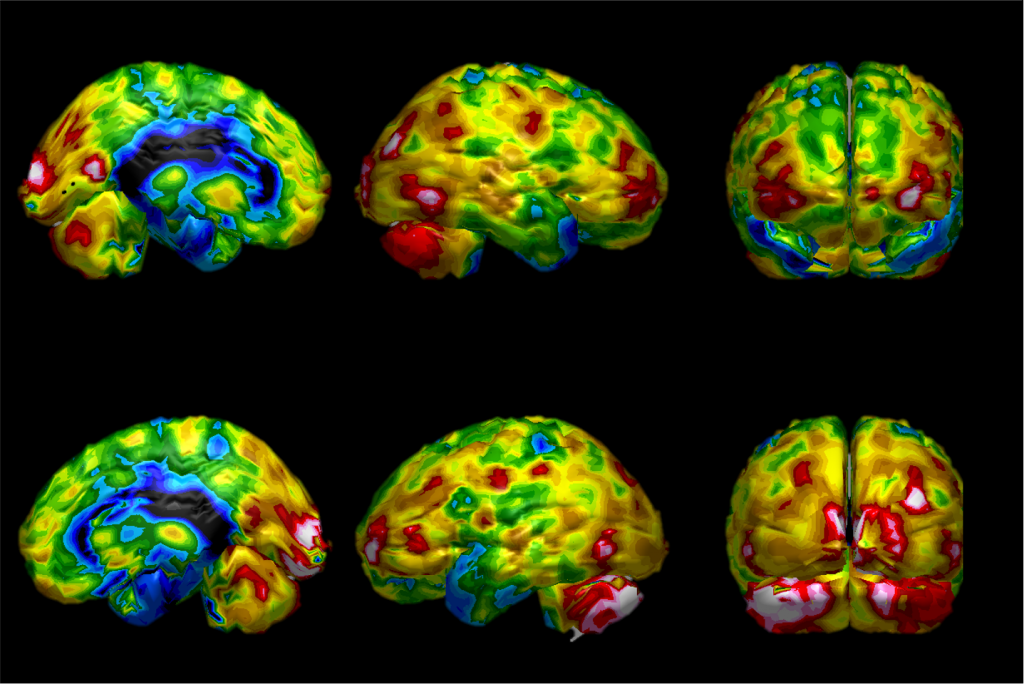
SPECT scan – enables doctors analyze the metabolic activity of portions of the brain
How do you treat a TBI?
One of the most promising treatments for brain injuries involves hyperbaric oxygen therapy (HBOT).
HBOT is a treatment where patients receive oxygen-enriched air in a special high-pressure chamber. The unique hyperbaric protocols were researched and tested for years at the Sagol Center for Hyperbaric Medicine and Research in Israel. They are now available at the Aviv Clinic, Jumeirah Lakes Towers (JLT), Dubai, U.A.E
HBOT has been shown to improve neuroplasticity and lead to the improvement of chronic impairments in patients with mild TBIs, even on brain injuries that are years old. HBOT also induces angiogenesis in the brain, the process by which new blood vessels form from existing ones. These structural changes in the brain can lead to improvements in thinking clarity, cognitive performance and overall quality of life!

Hyperbaric Suite, Aviv Clinics, Dubai.
Conclusion
While the name may sound scary, TBIs are both detectable and treatable, even years after they occur.
With the proper care, you can see improvements to your memory, cognitive function and overall quality of life!
For more information about Aviv Clinic’s personalized program and unique hyperbaric protocol, or to schedule an in person consultation, contact the clinic today.