Understanding Post-COVID Brain Fog: Causes and Treatment Options
For many, brain fog has become a prominent, lingering symptom after a COVID-19 infection. While we all experience occasional cloudy thinking when tired or under the weather, post-COVID brain fog persists for weeks or months after the initial illness.
With passing, short-term instances of brain fog, you can simply rest and feel like yourself in no time. However, when people experience lasting brain fog after COVID, recovery is rarely as swift or straightforward; individuals can continue to struggle with brain fog six months to a year or more after having COVID.
The PD World’s Aviv Clinics team is here to help make this journey less daunting. We believe knowledge is power, so our goal is to educate you on post-COVID brain fog causes and treatment options. Use this to help carve a more confident path forward for you or your loved one.
As you’re reading through this, keep in mind:
- Each person has a unique experience with COVID-19.
- Speaking with a doctor is a critical first step to diagnosing long COVID.
- Per the CDC, long COVID has alternative names. “People call Long COVID by many names, including Post-COVID Conditions, long-haul COVID, post-acute COVID-19, long-term effects of COVID, and chronic COVID.”
This article covers:
- What Is Brain Fog?
- What Causes Post-COVID Brain Fog?
- Is Brain Fog a Symptom of Long COVID?
- Is My Brain Fog Related to COVID-19?
- How Long Does COVID Brain Fog Last?
- What Are My Options for COVID Brain Fog Treatment?
- Long COVID Brain Fog Treatment FAQ
What Is Brain Fog?

Brain fog is a term that describes slow or sluggish thinking. Someone with brain fog may experience confusion, forgetfulness, and/or a lack of mental clarity. While many cases of brain fog are temporary, with COVID-19, brain fog can impact cognitive functioning long-term.
Of course, brain fog can occur for many other reasons. If you experience brain fog symptoms unrelated to COVID-19, we encourage you to explore our blog, where you can discover possible treatment options and insights into managing this condition.
How Common Is Post-COVID Brain Fog?
Multiple reports illustrate those with long COVID experience a variety of symptoms that may include brain fog.
- One study notes that, among post-COVID patients, “80% reported having experienced brain fog.”
- Harvard Health notes that 22% to 32% of patients who recovered from COVID-19 “find they still have brain fog as part of their experience of long COVID.”
Not only does the research show how the COVID-19 virus can affect our cognition, but it also illuminates the fact that anyone—no matter their COVID-19 history—can experience persistent brain fog.
How Does Brain Fog Affect COVID Patients in Everyday Life?
Living with severe and persistent brain fog after COVID is undeniably difficult. Though “brain fog” may sound trivial, the reality is often far from easy. People who experience long COVID brain fog often face many challenges, including:
- Difficulty performing tasks effectively at work
- Trouble engaging in everyday activities
- Changes in friend and family relationships
- Feelings of frustration or isolation
- Negative impacts on their overall quality of life
Acknowledging the seriousness of this condition is an important first step in addressing its challenges and finding solutions to mitigate its symptoms.
What Causes Post-COVID Brain Fog?
Stanford University School of Medicine researchers note brain fog from COVID-19 mimics the same cognitive issues caused by cancer chemotherapy (“chemo brain”). In both cases, excessive inflammation damages the brain cells and processes.
To better understand what goes on in cases of post-COVID brain fog, we can examine the link between:
- Where the COVID-19 virus attacks the brain
- How that impacted location in the brain affects long COVID symptoms
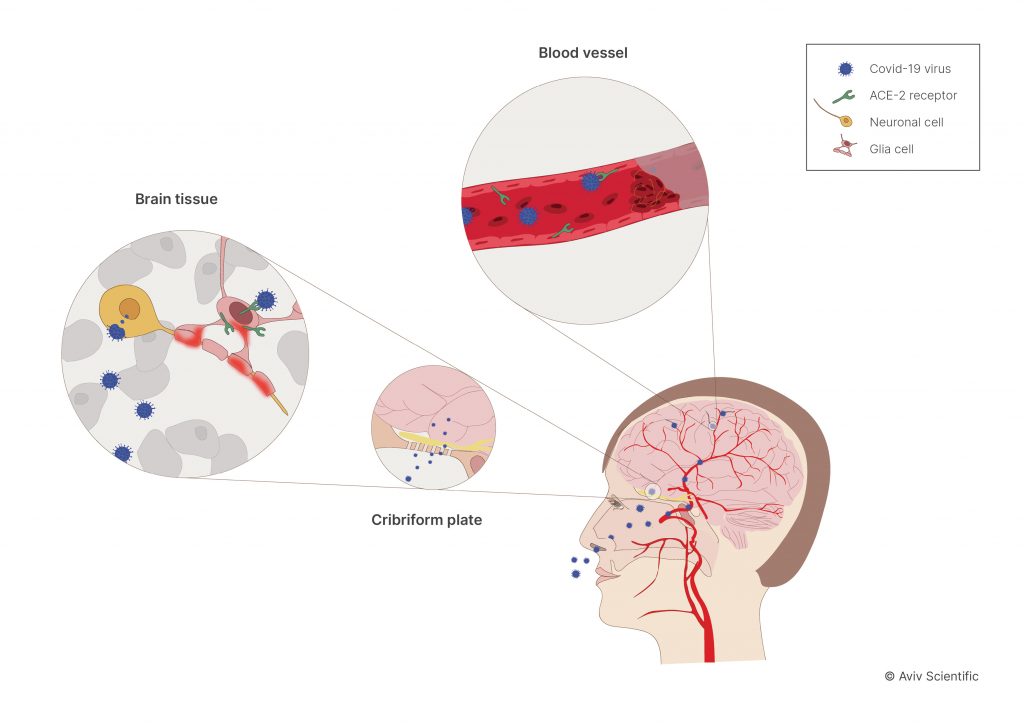
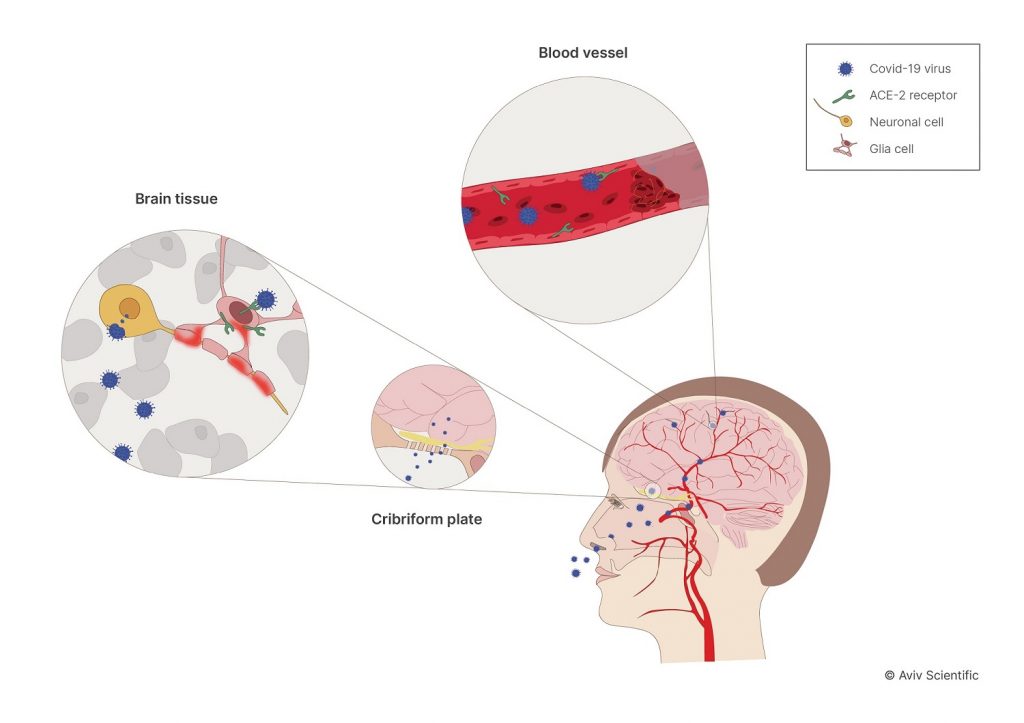
There are four main ways COVID-19 can attack the brain:
- Direct brain invasion: The virus travels through the nose and into the insula—a part of the brain involved in memory and executive function through its connection with the prefrontal cortex.
- Blood vessel injury: The virus may harm blood vessels that feed blood to the brain due to the “dysregulated cascade triggered by COVID-19 in the vascular system.”
- Dysregulated immune response: Damaged blood vessels caused by COVID-19 can slow the growth of cells, affecting the brain’s immune response.
- Cellular dysfunction: COVID-19 can trigger cell damage, “releasing pro-inflammatory factors.” This slows down the body’s response rate to infection, leading to high inflammatory conditions.
Is Brain Fog a Symptom of Long COVID?
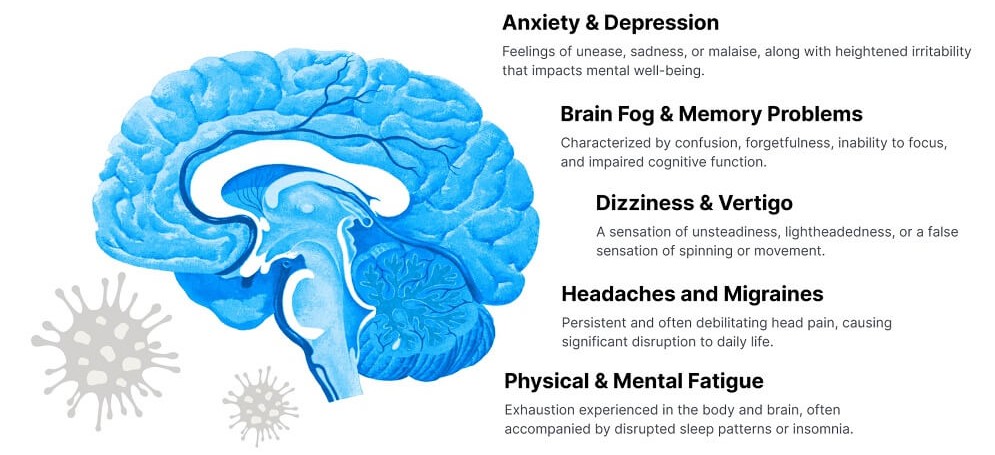
Yes, brain fog is a common symptom of long COVID—the CDC lists brain fog under its neurological symptoms. Brain fog from COVID-19 doesn’t necessarily need to manifest on a severe level; it can be subtle.
One study notes participants who had COVID and didn’t notice any cognitive problems still performed poorly on attention and memory tasks. “Testing showed that performance on an attention task was not as good among the group that had COVID compared with those who did not.”
Is My Brain Fog Related to COVID-19?
If you notice your cognition has not been the same since your COVID-19 infection, we recommend speaking with a physician. Your body and health background are entirely unique from other people’s. Therefore, it’s important to discuss your lingering symptoms with a healthcare professional.
Any potential long COVID brain fog symptoms warrant a personalized evaluation. The certified physicians at Aviv Clinics assess the following five areas to diagnose long COVID. Walking through these five areas enables your physician to provide the holistic approach your health deserves.
- Physical symptoms: Fatigue, cough, loss of taste or smell, labored breathing, joint/muscle pain, etc.
- Cognitive and psychological symptoms: Brain fog, anxiety, depression, sleep disturbances, headaches, etc.
- Lung symptoms: Shortness of breath, chest pain/tightness, etc.
- Cardiac symptoms: Heart palpitations, elevated blood pressure, decline in oxygen saturation, etc.
- Changes in the brain: Physical damage to brain structure and metabolism evident from extensive brain scans
How Long Does COVID Brain Fog Last?
As everyone’s bodies are different, there’s no set time limit for brain fog after COVID. Some research studies indicate most patients recover within six to nine months, with others experiencing COVID brain fog symptoms for two years or more.
How long a person experiences brain fog after COVID may depend on:
- The severity of their initial infection
- Their overall health status
- Individual differences in brain function and resilience
- Their age at the time of infection
One study found that the aging brain may experience the consequences of a COVID infection even longer. When measuring cognitive changes in older COVID patients, researchers found “an increase in risk of longitudinal cognitive decline” a year after the acute phase of the infection.
What Are My Options for COVID Brain Fog Treatment?

Rest assured—there are several ways to approach COVID brain fog treatment. The treatment options for long COVID brain fog should include activities and therapies that help address the root cause of symptoms.
Below, we offer tips on how you may be able to alleviate brain fog symptoms, including a unique evidence-based hyperbaric oxygen therapy protocol.
Addressing and Managing Brain Fog After COVID-19

Managing brain fog involves engaging in activities known to improve memory and thought processes. These activities may include:
- Exercising. The CDC states, “Physical activity can help you think, learn, problem-solve, and enjoy an emotional balance.” Participate in regular cardio and strength training exercises each week. Walk, jog, jump rope, or do resistance-band or body-weight exercises. The key is to stick to something you enjoy to help you stay motivated. One note: Your exercise regimen should be supervised by a clinician familiar with your condition, as overexerting yourself can make your symptoms worse, not better.
- Getting adequate sleep. Getting adequate amounts of sleep “fosters attention and concentration, which are prerequisites for most learning.” The Sleep Foundation recommends seven or more hours of sleep for adults.
- Eating a well-balanced diet. Aim for the MIND diet, which encourages you to consume diverse healthy foods. Designed to enhance brain health and reduce the risk of neurological conditions, the MIND combines the Mediterranean and DASH diets.
Unique Hyperbaric Oxygen Therapy (HBOT) Protocol for Long COVID Symptoms

Multiple studies reveal that a specific hyperbaric oxygen therapy (HBOT) protocol may help mitigate long COVID symptoms as part of a comprehensive treatment program. The unique treatment incorporates a rise and fall in oxygen levels during the session, which initiates the body’s self-healing mechanisms.
From clinical and qualitative evaluations of HBOT patients, researchers conclude there is hope HBOT can address some of the common symptoms, such as fatigue and brain fog:
“Long COVID-related fatigue can be debilitating…The results presented here suggest potential benefits of HBOT, with statistically significant results.”
New research suggests these results are more than temporary, demonstrating that “improvements gained by HBOT are persistent even 1 year after the last HBOT session.” The study showed significant long-term enhancements in:
- Quality of life
- Quality of sleep
- Psychiatric symptoms
- Pain symptoms
These enduring improvements offer hope for long COVID patients looking for relief, pointing to the potential long-term benefits of HBOT in managing the condition’s challenging symptoms.
For Fleury, a long COVID survivor of more than two years, the potential for relief from persistent fatigue, discomfort, and brain fog after COVID was well worth the 4,500-mile journey from the Netherlands to the U.S.
The holistic Aviv Medical Program can incorporate an evidence-based hyperbaric oxygen therapy protocol as part of each client’s customized treatment plan. Aviv Clinics’ team of certified physicians takes a three-step approach to their long COVID program:
- In-depth medical assessment: Conducting comprehensive testing (physical, cognitive, and neurological) and brain imaging
- Tailored treatment program: Creating a customized treatment plan based on your test results
- Post-treatment assessment: Administering a second round of testing to unveil findings/progress and make recommendations for ongoing improvement
Learn more about DP World’s Aviv Clinics’ long COVID approach.
Long COVID Brain Fog Treatment FAQ
Here are the answers to some common questions about long COVID brain fog treatment options.
Are there any medications that can help with post-COVID brain fog?
There are no specific medications that are approved for treating long COVID brain fog, but some medications—including antidepressants, anti-anxiety medications, and cognition-enhancing medications—may be prescribed to address individual or related symptoms.
Are there lifestyle changes that can help manage post-COVID brain fog?
Several lifestyle changes that support overall health can help manage brain fog in COVID patients. These include regular supervised exercise, getting enough sleep, adequate nutrition, and stress management techniques such as meditation and mindfulness practices.
When should I seek medical attention for post-COVID brain fog?
It’s a good idea to seek a medical evaluation if you experience COVID brain fog symptoms that persist or worsen over time, especially if your symptoms interfere with your quality of life. Your healthcare provider can evaluate your symptoms, conduct tests or scans, and make recommendations for treatment or management based on your individual needs and goals.
If you experience persistent brain fog after COVID, Aviv Clinics can help. Our physicians offer a complimentary consultation call to answer any questions and discuss your options.
The Bottom Line
Brain fog from COVID-19 can be difficult to live with. If you or a loved one suspects COVID-19 has left lingering cognitive issues, contact DP World’s Aviv Clinics Dubai.
Our team will offer the resources you need to learn more about how our team of physicians helps manage long COVID symptoms. Feeling your best cognitively and physically starts with us.
Breaking the Chains of Post-COVID Fatigue: How Hyperbaric Oxygen Therapy Helps You Get Your Life Back
Since the COVID-19 pandemic, many people have struggled with the aftereffects of the virus. Post-COVID fatigue is a condition characterized by nearly constant exhaustion and low energy levels, and it can affect people for a long time.
Fatigue is a common symptom of the COVID-19 virus. It can be more severe and last longer than the tiredness frequently experienced with other common or seasonal illnesses. While fatigue typically goes away after three weeks, some people experience feeling dull, tired, or drained for far longer periods of time.
If you’re living with post-COVID fatigue, you may have tried many different things to boost energy levels and start feeling like yourself again. Some remedies may seem to relieve the fatigue, only to stop working after a while.
Fortunately, there’s hope in a promising solution: hyperbaric oxygen therapy.

The Nightmare of Post-COVID Fatigue and Exhaustion
Dealing with extreme fatigue post-COVID is far from easy. Months after their initial infection with the virus, long-haulers may still wake up feeling as though they haven’t slept at all, and can’t seem to find the same energy they once had to make it through the day. At times, the exhaustion may seem never ending.
Post-COVID fatigue is more than just constant tiredness. Researchers have defined the condition as a “decrease in physical and/or mental performance” because of the COVID-19 virus.
Long COVID fatigue is also associated with other symptoms, including:
- Brain fog
- Cognitive impairments
- Reduced interest in relationships or activities
- Difficulty concentrating
- Insomnia and sleep disturbances
- Problems with memory
- Joint pain
Just as the virus does, fatigue related to long COVID affects a wide variety of people. Men and women of all ages can experience long-haul COVID. And while it’s not as common in children as adults, sudden extreme fatigue in pediatric COVID cases is possible. Research has found that “children may experience similar long COVID symptoms to adults.”

What Are the Causes of Post-COVID Fatigue?
The reasons behind post-COVID fatigue vary. However it’s likely that, most of the symptoms come from the body’s reaction to the virus. While the immune system is activated, it releases cytokines, which “promote inflammation and cause many of the classic symptoms of post-COVID fatigue (tiredness, aches and pains, malaise).”
These symptoms present various challenges. The impact of post-COVID fatigue on mental health and emotional well-being can make it difficult to complete daily tasks. Ultimately, it’s difficult to stay motivated when you feel tired all the time.
This has a strong emotional impact. Individuals living with Long COVID syndrome often feel frustrated and are strongly determined to find a solution.
When attorney and law firm COO Josh W. developed COVID pneumonia in 2021, it was only the beginning of his struggles. He suffered from excruciating nerve pain and other symptoms that left him unable to work for more than a few hours a day and distanced him from his family. He searched for months to find an effective treatment option for his symptoms. Now, he’s back on his “A-Game” at work and at home after completing the Aviv Medical Program.
The Quest for Solutions
For those who have searched for long-term solutions on how to deal with COVID fatigue, the journey to find relief can seem overwhelming. Remedies such as lifestyle changes, medications, and exercise may make a difference in how you feel day to day. However, they don’t address the condition at its core.
Those living with post-COVID fatigue can face challenges that are often not recognized or understood. Sometimes, it can feel like the constant tiredness may never go away. The good news is that there are ways to manage the effect of post–COVID fatigue that focus on the cause of the symptoms rather than just the symptoms alone.
Post-COVID Fatigue Recovery
Hyperbaric oxygen therapy (HBOT) is an innovative approach to address fatigue associated with long COVID. HBOT involves breathing pure oxygen in a pressurized chamber, allowing the body to absorb higher levels of oxygen than usual. This increase in oxygen helps to activate the body’s natural healing mechanisms, helping those living with fatigue post-COVID.
COVID-19 triggers internal inflammation as the body fights off the infection. In long COVID cases, this inflammation can persist, and inflamed tissues “tend to receive insufficient or extremely low levels of oxygen which delays the body’s healing process.”
HBOT is effective for its acceleration of oxygen to damaged or inflamed tissues. For those with post-COVID fatigue, this is especially beneficial, as “oxygen is a crucial factor in generating energy.”
Hyperbaric oxygen therapy can be beneficial for people living with long COVID for several reasons. In one landmark trial, long COVID patients who underwent a specialized two-month hyperbaric oxygen therapy program made notable improvements, including “reduced brain fog, improved memory and attention, more energy and less pain.”
The benefits of this therapy extend beyond even improvements in post-COVID fatigue. HBOT can also promote “recovery of cardiac function in patients with post-COVID syndrome.”
Pioneering research also discovered that HBOT can help to boost functional connectivity and “cognitive and emotional recovery” in the brain, which can support improvements in symptoms such as brain fog, concentration problems, and emotional regulation—all of which have ties to post-COVID symptoms, including fatigue.

Long COVID Treatment at DP World’s Aviv Clinics
DP World’s Aviv Clinics has helped numerous individuals along their post-COVID recovery journey. People living with long COVID symptoms can find relief through the Aviv Medical Program, a holistic and personalized program designed to improve brain and body performance. The program can include hyperbaric oxygen therapy, as well as cognitive training, dietary coaching, and physical training.
The clinics’ unique HBOT protocol employs a revolutionary oxygen process. The protocol uses oxygen fluctuations to increase the body’s capacity for absorption, allowing oxygen to more effectively reach the tissues that most need it.
Watch – Pieter’s Long COVID Symptom Recovery
Long COVID forced Pieter to spend the majority of his day in bed or on the couch. It took away his ability to run his coffee roastery business, be an involved dad and husband, and maintain an active and healthy lifestyle. However, a big leap of faith and a long journey from the Netherlands to the United States was exactly what Pieter needed to get his life back.
Six months after completing treatment at Aviv, his brain fog, fatigue and other long COVID symptoms are gone. He is doing all the things he loves, including training for a half marathon! “Here I am. I have my life back. I am full of energy.”
Healing and Reclaiming Your Life from Long COVID Fatigue
Those with post-COVID fatigue, even those who have dealt with the condition for months on end, have hope for healing. Through our comprehensive treatment programs, you can regain the energy and liveliness you used to have.
Aviv Clinics’ holistic program includes lifestyle changes, a focus on nutrition, and wellness support for people living with post-COVID fatigue. Discover how the unique program, including our advanced HBOT protocol, can help you experience improvement in long COVID symptoms.
“After weeks in hospital recovering from COVID-19, Patrick suffered fatigue, weakness, and shortness of breath that made it difficult to resume his usual outdoorsy and active lifestyle. Hear him describe how the treatment at Aviv Clinics, along with our multidisciplinary health team, not only helped him regain his physical fitness, but also provided support for his cognitive health.”
Watch: Aviv Clinics Helps Long COVID Sufferer to Return to his Active Lifestyle
Learn more about the personalized health program available at PD World’s Aviv Clinics and discover how we can help you heal from long COVID fatigue.
Long COVID Treatment: Your Comprehensive Guide to the Symptoms & Science
Living with long COVID can be a complicated and challenging journey. Each patient’s experience with the condition can be highly diverse, with symptoms that may be elusive, cyclical, and disruptive to many aspects of daily life. As the mechanisms behind the condition continue to be explored, these findings become instrumental in charting a course toward tailored, successful long-haul COVID treatment strategies.
Whether you’re currently facing the symptoms of long COVID or are searching for a more comprehensive understanding of the condition, information about the experience, the latest scientific insights, and current treatment options can be invaluable.
This guide is crafted to contain up-to-date, relevant information for those looking for long-term COVID treatment options on the path toward reclaiming their life.

What Is Long COVID?
Long COVID refers to a condition where individuals continue to experience, or even develop, symptoms and complications after an initial COVID-19 infection. While many people recover from COVID in a matter of days or weeks, others may develop lingering symptoms that can persist for months on end.
How Common Is Long COVID?
The prevalence of long COVID varies, but recent data indicates that “nearly one in five (19%)” of people who have previously reported a COVID-19 infection are still experiencing symptoms months after their initial exposure. This means “at least 65 million individuals worldwide” are estimated to be affected by long COVID.
Who Is Likely to Get Long COVID?
Long COVID can develop even in those with a mild or completely asymptomatic case of the virus. For some, the symptoms of long COVID may be more challenging than their initial acute infection.
Why this occurs is not fully understood. The exact cause of long COVID is still a mystery, but the condition has led to ongoing research and medical investigation to better understand its mechanisms and improve long-haul COVID treatment solutions.
How Long Does It Take to Recover from Long COVID?
Because each person’s experience with COVID-19 and long-haul COVID is unique, it’s important to reach out to healthcare professionals to discuss your symptoms. However, new research and innovative long COVID treatments can powerfully improve the outlook for long COVID patients.
How Has Long COVID Evolved?
The understanding and recognition of long COVID has evolved significantly since the early days of the pandemic. Initially, the focus was primarily on acute respiratory symptoms associated with COVID-19. The concept of persistent symptoms was not fully understood or acknowledged.
Over time, as more individuals recovered from the initial infection, it became clear that a subset of people continued to experience a range of lingering symptoms. This caused a shift from viewing the impact of the virus as short-lived to recognizing the complexity and persistence of symptoms as an ongoing condition that affects many individuals for months, and even years, after their first exposure.
Several factors contribute to this evolved understanding of long COVID, including:
- Public Awareness: More individuals, inside and outside the medical community, now recognize the prevalence of long COVID and its impact on those recovering from COVID-19.
- Diagnostic Criteria: The medical community worked to establish diagnostic criteria to aid in identifying individuals with persistent COVID symptoms.
- Recognition of Unique Experiences: It’s now known that long COVID encompasses a diverse array of symptoms that affect different systems of the body, widening the criteria to include individual experiences with the condition.
- Research and Studies: Ongoing research has deepened our understanding of long COVID by identifying common patterns of symptoms, risk factors, and potential mechanisms behind the development of the condition.
As the medical community continues collaborating and public awareness increases, our understanding and approach to long-term COVID treatment options should only evolve.
Long COVID Symptoms
Many of the common symptoms associated with long COVID present unique challenges to those living with the condition. In addition to the well-known respiratory symptoms of the virus, COVID long-haulers can also develop other troublesome symptoms, including:
- Fatigue: Chronic and profound fatigue or exhaustion can develop, and some cases may not be alleviated by rest.
- Shortness of Breath: Difficulty breathing or shortness of breath continues, even after recovery from the initial respiratory symptoms.
- Chest Pain: Discomfort or pain in the chest, often unrelated to heart issues, may persist.
- Cognitive Issues: These issues can include brain fog, difficulty concentrating, memory problems, and other cognitive challenges.
- Joint and Muscle Pain: Aches and pains in the joints and muscles can last or develop beyond the acute phase.
- Headaches: Persistent or recurrent headaches, sometimes resembling migraines, may be common in those with long COVID.
- Loss of Smell or Taste: Some individuals continue to experience anosmia (loss of smell) or dysgeusia (altered taste) for an extended period.
- Sleep Disturbances: Difficulty sleeping or changes in sleep patterns, either due to other symptoms or as a symptom in itself, is common.
- Gastrointestinal Issues: Persistent digestive symptoms, such as nausea, diarrhea, or abdominal pain, may develop or worsen with long COVID.
- Heart Palpitations: This includes irregular or rapid heartbeats that may continue after recovery from the initial infection.
Long COVID Symptoms and the Brain
Why Do Long COVID Symptoms Persist?
The persistence of long COVID symptoms is a complex phenomenon. Several potential explanations are considered:
- Ongoing inflammation
- Immune dysregulation
- Post-viral syndrome
- Autoimmunity
- Persistent viral presence
There’s still a lot to learn about how long [mitochondrial dysfunction] will last, but it will probably be tied to the level of microvascular change or blood vessel damage. The more blood vessel damage you have, the more [long COVID symptoms] you’re likely going to have. Also, the amount of real estate that those microvascular changes are occupying will probably dictate how long [symptoms] will last.
Fortunately for COVID long-haulers, treatment options developed to address the root cause of these symptoms show promise.
Post-COVID Fatigue

After a COVID-19 infection, many individuals find themselves battling persistent exhaustion and depleted energy levels. For many living with the aftereffects of the virus, post-COVID fatigue seems like it may never end.
One of the most common symptoms, post-COVID fatigue, is more than just a little tiredness. It can show up as a major decrease in physical and mental performance, affecting everything from emotional well-being to your ability to perform even basic daily tasks.
Finding relief from this intense level of fatigue can feel overwhelming, with many conventional remedies falling short. This can lead to a powerful sense of frustration and, for many, a determination to discover how to get rid of long COVID fatigue for good and find effective, long-lasting solutions.
What Causes Post-COVID Fatigue?
Though fatigue is a common symptom during and after a COVID-19 infection, the reasons behind its persistence vary. Ongoing research suggests it may be caused by:
- The body’s reaction to the virus
- Persistent inflammation
- The virus’ effect on mental health
Studies on post-COVID fatigue find that it’s largely caused by “any systemic inflammation…which activate[s] the innate immune system in the brain.” Lifestyle changes, medications, and symptom management may offer day-to-day relief. However, addressing the condition at its core requires a more comprehensive approach.
What Are the Treatment Options for Long COVID Fatigue?
If you’re yearning to reclaim your life from the grips of post-COVID fatigue, Aviv Clinics offers a beacon of hope through a holistic long-haul COVID treatment solution. The comprehensive Aviv Medical Program, which can incorporate a combination of lifestyle changes, cognitive training, nutritional focus, and a unique hyperbaric oxygen therapy (HBOT) protocol, can help you rediscover the vitality you thought was lost.
Long COVID Headaches and Migraines

Like everyday headaches, headaches experienced by individuals with long COVID can be intense and unyielding. Unlike typical head pain, people with long COVID experience them in addition to the many other symptoms associated with the condition. Those living with long COVID can experience seemingly mild headaches or debilitating migraines as often as daily. This can make the experience seem even more unbearable.
From cognitive impairments and difficulty concentrating to the notorious brain fog that clouds your mental clarity, long COVID headaches can worsen a set of already frustrating symptoms, extending even further into various aspects of everyday life.
Understanding the nuances of these headaches is crucial for those seeking answers and relief from the pain and disruption of this persistent symptom.
What Triggers Long COVID Headaches and Migraines?
Examination of the causes of long COVID headaches is essential for relief and provides insights into the broader landscape of the condition’s diverse symptoms. The persistent and often intense head pain linked to long COVID may be linked to several mechanisms, including:
- The virus’ impact on the nervous system
- Lingering inflammatory response
- Changes in blood flow and oxygen supply to the brain
- Neurological complications
- A persistent heightened immune response
Ultimately, how the virus impacts various body systems may play a role in lingering headaches associated with long COVID.
How Long Do Headaches Last Post-COVID?
The duration of post-COVID headaches and migraines can vary widely among individuals, with some experiencing recurring headaches for weeks or months. While some people experience headaches for a relatively short period, others can grapple with intense headaches for an extended duration, underscoring the importance of effective long-term COVID treatment options.
Understanding the causes and duration of long COVID-related headaches is only the beginning. Thanks to breakthroughs in long COVID treatments, many individuals can take steps toward reclaiming their lives from the clutches of persistent head pain.
Long COVID Vertigo

For many, vertigo is another ongoing symptom that adds layers to the challenges of long COVID recovery. In addition to chronic pain, brain fog, and fatigue, as many as “60% of patients [report] the presence of vertigo or dizziness” in varying levels of severity.
Understanding the Link Between Long COVID and Vertigo
Vertigo—the sensation that the world is spinning or the ground feels unsteady—can be a lingering symptom in the aftermath of a COVID-19 infection. Several mechanisms may trigger this sensation in COVID long-haulers, including inflammation and changes in the brain.
Recognizing vertigo symptoms—including spinning sensations, a loss of balance, visual disturbances, and nausea—is pivotal for early intervention. Exploring the presence of neurological inflammation may be a key component to consider during the evaluation and diagnosis process, which can help connect patients to timely and targeted care solutions in the face of long COVID-related vertigo.
Long-Term COVID Treatment for Vertigo Symptoms
Traditional approaches to managing vertigo involve several different treatment and coping strategies, such as:
- Medical interventions
- Medications
- Lifestyle modifications
- Therapy
However, cutting-edge solutions for long COVID vertigo get closer to the core of the issue by addressing changes in the brain and vestibular system—both areas shown to be impacted by the virus. Drawing from ongoing research in neuroscience, targeted, holistic interventions could be the key to finding lasting relief from post-COVID vertigo.
Post-COVID Brain Fog

Brain fog, a symptom that involves sluggish thinking, confusion, and forgetfulness, is common in those who develop an acute COVID-19 infection. However, when it lingers for months after initial exposure—as it does in many who experience long COVID—the persistence can be exhausting.
As many as 80% of people recovering from COVID report brain fog as a symptom that just doesn’t seem to go away. While the cognitive impact of the COVID-19 virus affects individuals differently, it’s common to experience:
- Poor concentration
- Mental fatigue
- Slow thinking
- Unexplained forgetfulness
- Irritability
- Disorganized thoughts
The connection between brain fog and a previous COVID-19 infection illustrates the virus’ impact on the brain. Most notably, brain fog is a symptom that can develop in individuals with long COVID regardless of whether they initially experienced a mild or even asymptomatic case.
How to Get Rid of Long COVID Brain Fog
Among the available options for COVID long-haulers, treatment solutions may include:
- Engaging in exercise
- Maintaining a well-balanced diet
- Getting adequate sleep
These solutions can help address the root cause of brain fog and bolster memory and various thought processes. Suppose you suspect your brain fog is related to COVID-19 and its lingering effects. In that case, a more holistic long COVID treatment solution may help manage the symptoms by promoting healing at the cellular level.
Cognitive Impairment & COVID-19

As we continue to understand the long-term effects of COVID-19, research reveals a concerning connection between the virus and persistent neurological issues. Beyond respiratory symptoms, a substantial number of individuals endure cognitive impairments long after their first infection.
Does COVID Affect Long-Term Cognitive Function?
Studies have shown that COVID-19 has implications for long-term cognitive functioning, as those recovering from the virus can continue to experience cognitive challenges for weeks and months after exposure. In some patients, these challenges may last for years.
In fact, some of the most “common, persistent and disabling symptoms of long COVID are neurological.” These symptoms can persist for a long time and can develop in individuals regardless of age or the severity of their initial infection.
Is Long COVID Cognitive Decline Permanent?
The duration of cognitive impairment after COVID-19 can vary, but evidence suggests that long-term challenges may not be permanent; they can improve over time through holistic, long-term COVID treatments that aim to address the root causes of the symptoms.
Specialized interventions grounded in medical science can promote healthy tissue regeneration in the brain and body by triggering the body’s innate healing mechanisms. Clinical trials have demonstrated the efficacy of hyperbaric oxygen therapy (HBOT) in facilitating recovery and promoting overall wellness in those grappling with enduring cognitive symptoms of long COVID.
Comprehensive long-haul COVID treatment programs that include HBOT and lifestyle changes such as clean diets, regular exercise, and stress management may be the key to addressing long COVID’s neurological impact.
Myocardial Function in Post-COVID-19 Patients

Long COVID can affect various internal systems in people living with the condition, including cardiac health. Many COVID long-haulers suffer from cardiac dysfunction, putting them at increased risk for several disorders.
The exact mechanisms through which COVID-19 affects the heart are complex and involve a variety of factors. The virus may cause inflammation throughout the body, including the heart muscle. The inflammation, coupled with the potential for blood clotting issues associated with the virus, may contribute to cardiac complications.
Pioneering Research on Myocardial Function for COVID Long-Haulers
A groundbreaking study conducted by the Sagol Center for Hyperbaric Medicine and Research at Shamir Medical Center and Tel Aviv University sheds light on the effectiveness of a unique hyperbaric oxygen therapy (HBOT) protocol in addressing cardiac dysfunction in post-COVID patients.
This study, published in Scientific Reports, shows promise in enhancing cardiac function for individuals experiencing long COVID symptoms. The results demonstrated that the unique HBOT protocol, when administered regularly over the course of several weeks, effectively restored ventricular systolic function in post-COVID patients. This discovery offers hope and insight into potential avenues for recovery.
According to Dr. Shai Efrati, a researcher on the study and chair of Aviv Scientific’s Medical Advisory Board:
“This HBOT protocol has already shown to be effective in improving neurocognitive function in post-COVID patients, and now, we show it can also improve cardiac function in post-COVID patients. People with post-COVID are suffering with lingering symptoms and we’re still learning more about the lasting effects of COVID-19. With this study, we are able to provide hope for post-COVID patients that they didn’t have before.”
Read more from the study here.
The Aviv Medical Program: Treatment for Long COVID Symptoms

DP World Aviv Clinics Dubai stands at the forefront of addressing the complexities of long COVID symptoms, offering a groundbreaking approach to long-term COVID treatment through the Aviv Medical Program.
Long-haulers dealing with seemingly unending symptoms can now find relief through this science-backed treatment, which can involve a combination of specialized hyperbaric oxygen therapy (HBOT), cognitive and physical training, and nutritional coaching—all tailored to individual patient needs and health goals.
Comprehensive Long-Haul COVID Treatment
The Aviv Medical Program follows a structured process: An in-depth medical assessment, a tailored treatment program, and a post-treatment assessment to measure progress and recommend further improvements. The holistic approach aims to address the underlying causes of long COVID symptoms, offering a beacon of hope to those navigating the challenges of persistent illness.
To provide a comprehensive, personalized treatment program for each patient, DP World’s Aviv Clinics boasts a multidisciplinary team including:
- Physicians
- Neurologists
- Physiologists
- Neuropsychologists
- Nurses
- Nutrition experts
Several studies highlight the efficacy of the therapies used in the program for improving cognitive, cardiac, psychiatric, fatigue, sleep, and pain symptoms associated with long COVID.
A Unique HBOT Protocol
Among other interventions, the Aviv Medical Program can include a unique hyperbaric oxygen therapy protocol as one of the treatments for enduring long COVID symptoms. In traditional hyperbaric oxygen therapy, individuals breathe 100% pure oxygen at a higher-than-normal atmospheric pressure. This prompts the body to increase oxygen saturation in the blood and tissues, which supports tissue repair and regeneration.
DP World’s Aviv Clinics offers a unique HBOT protocol that leverages the Nobel-prize-winning discovery of the hypoxic response to further trigger the body’s natural healing mechanisms. Essentially, the hyperoxic-hypoxic paradox sparks the body’s healing potential by fluctuating oxygen levels, challenging the body to work harder to adapt and recover as a response to a perceived lack of oxygen.
Learn more about treatment for long COVID symptoms.
Recovering from Long COVID
“My life today is back to normal, but on a higher level than before”
“I say this clinic saved my life and improved my life. I’m forever grateful for that.” says Patrick Bol, who overcame the symptoms of long COVID and regained his peak performance after undergoing the Aviv Medical Program.
Josh’s Life-Changing Long COVID Recovery
When attorney and law firm COO Josh developed COVID pneumonia in 2021, his struggles were only beginning. He suffered from excruciating nerve pain and other symptoms that left him unable to work for more than a few hours a day, distanced him from his family, and contemplating suicide. Fortunately, Josh is back on his “A-game” at work and with his family after completing the Aviv Medical Program.
Danielle’s Long COVID Recovery Story
Long COVID caused an active mom who had superb blood pressure, worked out three times a week, and ran half-marathons to transform into a parent who struggled to make lunch for her children due to confusion, numbness in her extremities, vision troubles, and dangerously high blood pressure. Danielle G. felt hopeless—until she found Aviv Clinics.
Find Long COVID Relief at DP World’s Aviv Clinics Dubai

If the lingering symptoms of long COVID impact your daily life, there is hope. At DP Aviv Clinics, our dedicated team of professionals collaborate to create a personalized long COVID treatment program designed to help you on your road to recovery.
Backed by scientific research, this comprehensive approach can help address the cognitive, physical, and mental symptoms of long COVID and help you reclaim your life. Take the first step toward getting your life back on track after a COVID-19 infection.
If you’re suffering from long COVID, contact us for help. We can help you get your life back!
Long COVID Explained: The Symptoms and Why They Stick Around
Last updated: January 15, 2024
Millions of individuals who have tested positive for COVID-19 continue to experience ongoing health issues, clinically known as long COVID. If you’re one of these people, the Aviv team is here with research-backed information on what this means and what you can do.
While there is still uncertainty surrounding COVID-19 complications and their long-term side effects, there have been extensive studies conducted that offer insight into:
- Post COVID symptoms
- How long COVID can impact your body and lifestyle
- Treatment methods that can help mitigate long-haul COVID effects
Below, we provide all the details you need to attain a holistic understanding of how long COVID impacts your body and promising treatment plans that can help you get back to optimal health. As you’re reading through this, keep in mind:
- Each person has a unique experience with COVID-19.
- Therefore, speaking with a doctor is an essential first step.
- Several alternative terms are used for long COVID, such as post-COVID, long-haul COVID, post-acute COVID, and chronic COVID.
How the CDC and WHO Define Long COVID
- The Centers for Disease Control and Prevention (CDC) defines long COVID as a condition where individuals experience long-term effects of COVID-19.
- The World Health Organization (WHO) defines long COVID as persistent symptoms more than 3 months after the acute infection, that continue, not relapse, that have been reoccurring and there is no other explanation for those symptoms.
- Anyone who has been infected with COVID-19 can develop long COVID. Approximately 30% of COVID-19 patients report having symptoms of long-haul COVID.
The numbers of people affected long term are high
The WHO had a definition of long COVID over two years ago. That means, from nearly the beginning, these health organizations studying the virus were seeing long-term side effects and symptoms of impairment from having COVID-19.
You aren’t alone if you don’t feel like yourself after having COVID-19.
- Approximately 30% of COVID-19 patients report having symptoms of long-haul COVID.
- 20-50% of patients with 1 or more features 3-6 months post COVID, receive a long COVID diagnosis.
- 11-20% of children have lingering symptoms at 14 weeks post COVID.
For a comprehensive understanding of what long-haul COVID is, let’s flesh out the differences between COVID and long COVID:
Acute COVID:
- Individuals experience COVID-19 symptoms for up to four weeks, starting from the onset of illness.
- Subacute is where COVID-19 symptoms are noticed up to 12 weeks, and the virus can still be found in the body.
Long COVID:
- Individuals experience COVID-19 symptoms for an average of three months from the onset of illness.
- Long-haul COVID symptoms may begin after initial recovery from acute COVID or persist from the initial illness.
- Long COVID symptoms cannot be explained by an alternative diagnosis.
Understanding the Symptoms of Long-Haul COVID
The Aviv medical staff primarily explores the four key areas from this long-haul COVID symptoms list to diagnose long COVID.
Physical Symptoms:
- Fatigue
- Dyspnea (labored breathing)
- Chest pain or tightness
- Cough
- Dysgeusia (loss of taste)
- Anosmia (loss of smell)
- Joint or muscle pain
Cognitive & Psychological Symptoms:
- Memory decline
- Attention and concentration difficulties
- Brain fog
- Anxiety
- Depression
- Sleep disturbances
- Headaches
- Generalized disabling pain
- Lung Symptoms
- Shortness of breath
- Chest pain or tightness
Cardiac Symptoms:
- Myocarditis (inflammation of heart muscles)
- Heart palpitations
- Shortness of breath
- Elevated blood pressure
- Drops in oxygen saturation
If you are experiencing long COVID symptoms,
contact our team of certified medical professionals today – click here.
The Hard Truth: Long COVID & Brain Injuries
COVID-19 essentially impacts the brain. This is why the majority of long COVID symptoms are cognitive and may lead to brain injuries, depending on how severely your body gets affected by the virus.
According to Dr. Mohammed Elimar, MD, FACP, although there are no patterns between the severity of COVID-19 and the likelihood of receiving long COVID, there are patterns between:
- Where the virus attacks in the brain
- How that location in the brain impacts long COVID symptoms
Here are four ways that connection can manifest:
1. Direct Brain Invasion
The COVID-19 virus travels through the nose, into the olfactory sensory neurons, and into the frontal lobe of your brain called the insula. The olfactory neurons manage taste and smell, while the insula oversees memory and executive function. Depending on where the virus attacks and the level of damage it creates, an individual may experience prolonged COVID symptoms.
For example, when the virus significantly attacks your olfactory nerves, this may induce a loss of taste and smell. This is why these symptoms are such a strong indicator of the virus.
2. Blood Vessel Injury
Studies show COVID-19 can destroy blood vessels that feed blood to the brain. As the virus circulates throughout your bloodstream, the inner blood vessel lining is susceptible to damage. When the inner lining deteriorates, this allows the virus to: Seep into the tissues, or inhibit blood flow to the brain. Both can cause brain injuries. And depending on where those injuries occur, specific brain functions (memory, concentration, etc.) may decline more rapidly than normal.
3. Dysregulated Immune Response
Damage to the inner blood vessel lining can also inhibit the growth of cells—the exact opposite of what our immune system should be doing. Dysregulated immune responses are common in those with severe cases of COVID-19.
When the body cannot adequately produce a normal immune response, it either: Underreacts to foreign invaders, causing viruses to spread quickly; or oerreacts to foreign invaders, causing the immune cells to attack even healthy cells, tissues, and organs.
4. Cellular Dysfunction
On a cellular level, COVID-19 can affect metabolic function through the mitochondria. This cell damage slows down the body’s response rate to infection, leading to high inflammatory conditions.
So how long will patients have to deal with COVID symptoms?
According to Dr. Mohammed Elimar, MD, FACP, the answer isn’t available.
But a key guiding factor is the extent of blood vessel damage.
Dr. Elimar further explains:
“There’s still a lot to learn about how [mitochondrial dysfunction] will last but it will probably be tied to the level of microvascular change or blood vessel damage. The more blood vessel damage you have, the more [long COVID symptoms] you’re likely going to have. Also, the amount of real estate that those microvascular changes are occupying will probably dictate how long [symptoms] will last.”
Aviv Clinics’ Treatment for Long COVID Symptoms
Long COVID is a complex disease.
Finding a treatment plan that will work for you may take some time.
Because there is no one-size-fits-all approach, speaking with a medical professional is essential.
The right physician will take a holistic approach. Due to the complexity of long COVID, it’s important to find a treatment program that:
- Is rooted in data and research
- Offers a comprehensive assessment process
- Connects you with a diverse medical team
Aviv Clinic’s team of certified physicians achieves all of the above to ensure you’re being provided with a tailored treatment plan that works for you. We connect our patients with a team of physicians, neuropsychologists, physiotherapists, nurses, and more to provide a multidisciplinary health plan – The Aviv Medical Program.
Our post-COVID symptom treatment plan can be broken down into three parts:
- In-depth medical assessment:
Leveraging advanced brain imaging, our clinical team conducts physical, cognitive, and neurological exams to gain a thorough understanding of your health. - Tailored treatment program:
Based on your assessment, our medical team crafts a personalized treatment plan, based on the results of your assessments, that includes hyperbaric oxygen therapy sessions, brain and physical training and a nutritional regimen designed to maximize the body’s healing process. - Post-treatment assessment:
Our team initiates another round of tests to assess your progress and unique findings on any cognitive and physical improvements.
Watch Patrick’s Successful Journey in Fighting Long COVID
First Long COVID treatment backed by clinical trials – help heal the brain to reduce or eliminate the symptoms of long COVID
The Aviv Medical Program is backed by extensive clinical research.
The most recent study confirmed that the COVID-19 virus can cause chronic brain injury affecting regions of the brain responsible for cognitive function, mental status and pain interpretation.
In the published study, patients treated with the Aviv protocol had significant improvement in their global cognitive function and cognitive improvement in the damaged brain regions responsible for attention and executive function. Significant improvement was also demonstrated in the energy domain, sleep, psychiatric symptoms and pain interference. The beneficial effects of the unique treatment protocol can be attributed to neuroplasticity and increased brain perfusion in regions associated with cognitive and emotional roles.
Read more about the Aviv Medical Program for Long COVID
Dr. Shai Efrati of summarizes the results of a study by saying:
“HBOT can induce neuroplasticity and improve cognitive performance, psychiatric state, assist with fatigue, aid sleep and relieve pain symptoms for patients suffering from post covid 19 condition. The beneficial effect can be attributed to increased brain perfusion and brain plasticity in regions associated with cognitive and emotional roles. HBOT can repair brain network connectivity and activity, and improve cardiac functions in post covid patients suffering from reduced GLS.”
WebMD recently published the research of Dr. Efrati, noting the clinical trial that began in December 2020 shows great potential for Long COVID patients whose issues are connected to brain tissue damage.
Maximize Your Health and Performance with Aviv
Though COVID-19 may have brought ongoing health challenges, the Aviv team is here to help you and your loved ones get back to optimal health. Aviv delivers a personalized protocol to enhance your mind and body and feel like yourself again.
Learn more about our team, contact our clinic to schedule a free phone consultation. Maximizing your health and performance begins with Aviv.
Cognitive Impairment & COVID-19: What We Know So Far
There’s a lot that we still don’t know about COVID 19, especially when it comes to the long-term effects. However, emerging research suggests a troubling new link between the Coronavirus and long-term neurological dysfunction. Many “COVID long-haulers” continue to experience headaches, dizziness, fatigue, and brain fog even weeks after recovering from the Coronavirus. Research also suggests links between the virus and increased risk for strokes, which is concerning for older adults or anyone who already had an increased risk.
If you’ve been feeling lost and dazed since recovering from the Coronavirus, you’re not alone. But don’t despair. In this article, we’ll address the potential neurological effects of COVID-19, along with our best advice for COVID long-haulers.
What is a “COVID long-hauler”?
“COVID long-hauler” is a new term used to describe the growing number of people who continue to experience symptoms of the Coronavirus weeks after recovering. Common complaints among long-haulers include respiratory problems like a persistent cough or shortness of breath. Neurological problems are also common, including headaches, fatigue, loss of taste/smell, and the now-infamous “Covid brain fog”.
Long-haulers are a diverse group, and anyone can become one, young or old. It’s not unusual for someone to report feeling like they’re “in a fog” or “stuck in a daze” even weeks after testing negative for the virus. Some people may be plagued by COVID fatigue or headaches, while still others can’t taste their favorite foods.
You don’t need to have been hospitalized to be a COVID long-hauler, either. Even mild cases can lead to these unpleasant after-effects, which is why you still don’t feel like your old self even after a minor bout with the virus. It’s unclear exactly why some people become COVID long-haulers while others experience no ill effects. But researchers are working hard to gain a greater understanding of the risk factors involved.
How COVID affects the brain
Did you know that when it comes to COVID, losing your sense of smell is actually a neurological problem? It’s true. The Coronavirus can affect the olfactory nerve connecting your nose to your brain, which inhibits your sense of smell. It was one of the earliest signs that COVID could affect the brain. While we still need more research to determine the full extent of COVID’s neurological effects, preliminary studies have revealed a connection between the virus and impaired cognitive performance.
In the study, a group of COVID-19 patients between the ages of 30 and 60 underwent a series of neuropsychological tests to assess various functions of their brains, including memory function, processing speed, and executive function. The COVID-19 patients experienced inhibited cognitive function when compared to a healthy test group, and they especially struggled with sustaining attention on the tests, providing us with evidence that the “COVID brain fog” is a real phenomenon.
Further studies have also provided us with links between COVID and headaches and COVID and strokes, giving us a greater understanding of how the virus can impact the brain.
The inflammation connection
Interestingly, COVID patients also exhibit high levels of inflammation in their blood. That’s not surprising since inflammation is one of the immune system’s natural responses to threats. In low levels, inflammation is a good thing; it’s a sign that your body is addressing the problem as intended. But as with everything in life, balance is key, and excessive inflammation can wreak havoc on your health.
One of the symptoms associated with coronavirus is a “cytokine storm”, an overactive immune response that skyrockets inflammation levels. Cytokine storms have been associated with reduced oxygen in the blood and other respiratory problems caused by COVID-19. They’ve also been linked to neurological problems, like brain fog, fatigue, or the stabbing headaches associated with the virus.
COVID and Strokes
While it’s still unclear exactly why COVID increases the risk of ischemic strokes (blood clots) in some people, inflammation could play a part. Chronic inflammation has long been linked to an increased risk of stroke, which could explain why the aging population is more susceptible.
Picture two highways. One highway is smooth and freshly paved without any potholes or blemishes. It’s easy for traffic to flow through this highway on a consistent basis, and traffic jams are uncommon. On the other hand, the second highway is littered with potholes, cracks, and closed lanes, all of which make it difficult for traffic to flow even on a good day. Now, which highway do you think will fare better when a snowstorm strikes?
The highways in this analogy are your blood vessels, and the flow of traffic is your blood cells. The snowstorm is, of course, COVID-19. Having high levels of inflammation in your body makes it easier for the blood to clot, which can ultimately lead to strokes. This is also why those with pre-existing conditions are hit hard by the virus — because their immune systems are already inflamed from fighting other problems.
How to combat inflammation
Because COVID patients almost always exhibit higher levels of inflammation in their blood, having low inflammation levels in your body can help combat the severity of the virus. Eating a clean diet, exercising regularly, getting plenty of sleep, and avoiding stress keeps inflammation levels low, which can help COVID long-haulers find relief. Avoiding stress is especially key, although that’s often easier said than done.
If you’re feeling stressed because of the pandemic, you’re definitely not alone. If the constant barrage of information from the news and social media is stressing you out, try unplugging for a while. Fire up the iPad for a chat with your grandkids, or head outside for a (socially-distanced) walk in the fresh air. While it’s important to stay informed, it’s also important to take care of your mental health.
Could getting vaccinated help a COVID long-hauler?
What about the Coronavirus vaccine? If you’re a COVID long-hauler plagued by brain fog or headaches, could getting vaccinated provide relief? Unfortunately, probably not. The purpose of the vaccine is to train your body’s immune system to fight against the Coronavirus. It’s meant to be used as a preventative measure. It’s not a cure, and it’s not a way to mitigate the virus’s after-effects. That’s no reason not to get vaccinated, however.
Even if you’ve already contracted the virus, the vaccine can prevent you from getting it a second time, which can minimize your risk of suffering long-term side effects. And if you’ve never contracted the virus before, getting vaccinated can ensure that you never have to deal with long-term side effects in the first place.

When to see a doctor about your long-term Coronavirus symptoms
If you’re struggling with long-term COVID neurological symptoms, you don’t need to suffer alone. Whether you’re being plagued by fatigue, brain fog, dizziness, headaches or loss of taste, any problem that impacts your quality of life is worth bringing up to your doctor.
Although your doctor may not have all the answers yet, they’ll do everything they can to help you cope with your symptoms. There’s also the possibility that your symptoms may not be caused by COVID at all, but by another health condition instead. Never hesitate to seek help when you need it, especially when it comes to your cognitive well-being.
The bottom line
While we still need more research to determine the full extent of the Coronavirus — especially when it comes to long-term symptoms — anyone of any age can minimize the damage caused by COVID simply by practicing healthy lifestyle habits and keeping your inflammation levels low. Taking care of your body inside and out is crucial not just for fighting COVID, but for any health condition you may encounter.
You can also minimize your chances of contracting the virus by continuing to follow the CDC guidelines of mask-wearing, social distancing, and getting vaccinated when you can. Above all else, staying calm and optimistic is one of the most important things you can do in the face of the pandemic. So do your best to stay positive.