Does High Blood Pressure Cause Memory Loss?
We all know that high blood pressure can cause a host of other health issues, although most of us are unaware that high blood pressure can cause memory loss. Cognitive decline is a side effect that isn’t always discussed. But having high blood pressure can directly affect your cognitive function, causing problems like brain fog and forgetfulness, as well as severe cognitive issues like vascular dementia.
Nearly one in three Americans and two-thirds of adults age 60 and older have high blood pressure, making it one of the most notorious killers in the United States. Fortunately, there are actionable steps you can take to manage your blood pressure, no matter your age.
Treatment options, such as the research-based hyperbaric oxygen therapy (HBOT) protocol available at Aviv Clinics, target associated health challenges like post-stroke, and age-related cognitive decline. Keep reading to learn more about how high blood pressure can cause memory loss, plus what you can do.

What Is High Blood Pressure?
Also called hypertension, high blood pressure occurs when the force of the blood pushing against the walls of your blood vessels is too high.
Every blood vessel in your body requires a certain amount of pressure to stay intact. High blood pressure may damage arteries, making them less elastic. Lower elasticity slows blood and oxygen flow to vital areas of the body. Health problems happen when your blood pressure wanders outside the acceptable range.
The higher your blood pressure, the greater your risk for health problems like heart disease, heart attack, and stroke. It also increases your risk of cognitive problems later in life.
What’s An Acceptable Blood Pressure?
Normal blood pressure levels differ for every person and depend on age, weight, and other factors. According to the American College of Cardiology and the American Heart Association:
- Stage 1 hypertension occurs at 130/80 mm Hg
- Stage 2 hypertension occurs at or above 140/90 mm
High blood pressure is unique because it doesn’t present symptoms on its own. The only way most people even discover that their blood pressure is high is when something more serious happens, like a clot. The best way to learn whether your blood pressure is at a healthy level is to measure it with a blood pressure machine at a doctor’s office, pharmacy, or on a home blood pressure machine.
Tip: A home blood pressure device is a worthwhile investment to monitor your health. Take your measurements at the same time every day for consistency, as your blood pressure will naturally rise and fall during the day.

How Exactly Does High Blood Pressure Impact Memory Loss?
The brain receives roughly 20–25% of the body’s blood supply. When high blood pressure causes the supply to decline, the brain lacks the nutrition needed to perform at optimal levels.
High blood pressure can also harm the tiny arteries that feed “white matter,” or the wire-like cells that transfer information to different brain areas. These issues may manifest with memory problems, confusion, lack of concentration, and other side effects.
Research Studies
Age-related cognitive decline studies show having high blood pressure during midlife can affect cognition later in life. We’ll let these research studies help clear the fog on the link between the brain and blood pressure:
- In this study, men at an average age of 78 years logged their blood pressure. After adjusting for biases like prior education and age, the men who performed the most poorly on the test were those who had experienced high blood pressure in middle age. This suggests a direct connection between hypertension and cognitive decline later in life.
- More recent studies have helped to reaffirm the connection between hypertension and cognitive decline. Researchers found mental processing speed and executive function were the top two cognitive skills most affected later in life.
Vascular Dementia
High blood pressure directly increases the risk of developing vascular dementia—a type of dementia caused by blood flow problems in the brain from strained blood vessels. The strain on the blood vessels makes it difficult for the brain to get the oxygen needed to function correctly.
Fortunately, vascular dementia symptoms can be improved through hyperbaric oxygen therapy (HBOT), such as the type available at Aviv Clinics in central Florida. HBOT works by delivering oxygen directly to the brain in a pressurized environment. The direct supply of oxygen allows the damaged blood vessels in your brain to heal, helping you regain some cognitive functions.
How Can You Manage High Blood Pressure?
While medication is often the first thing people think of, investing in your health via lifestyle choices and research-backed therapies is really the best medicine for managing high blood pressure.
The absolute best things you can do for your high blood pressure and brain health are the following:
- Eat a clean diet of whole foods to promote your gut health.
- Exercise to help maintain or manage your weight.
- Get enough sleep by establishing a bedtime routine, working up a sweat, and turning off the TV.
- Engage your mind by gardening, reading, or even playing a video game with your kids or grandkids.
- Reduce and manage your stress levels with activities like yoga or meditation. Practicing mindfulness meditation can help you stay grounded in the present moment and reduce stress.
- Seek unique and comprehensive therapies, such as hyperbaric oxygen therapy (HBOT). Research-backed HBOT programs, such as the one offered as part of the Aviv Medical Program, encourage damaged vessels to heal and cognitive functions to improve.
Aviv’s unique protocol may include HBOT, along with cognitive training, dietary coaching, and physical performance training. This holistic approach has been key to restoring our patients’ optimal health.
Find Hope and Healing with Aviv
While high blood pressure is dangerous, especially later in life, it is possible to manage it. It’s never too late to start, even after a cognitive decline diagnosis.
If you’d like more guidance, reach out to the Aviv Clinics team.
5 tips for sound sleep and a healthy brain
It doesn’t matter what age you are, getting a good night’s rest is essential for your physical and mental health. Taking the time to recharge every night is especially vital because sleep and brain health are closely related. However, as we age, sleep doesn’t always come as easily as it used to.
In a 2003 poll, the National Sleep Foundation found that over 48% of older adults experience symptoms of insomnia more than twice a week, and the National Institute on Aging reported that insomnia is one of the most common problems experienced by adults aged 60 and over.
Insomnia and sleep disruptions have been known to worsen health conditions like Alzheimer’s disease and increase your risk factors for developing other health problems, including heart disease, Type-2 diabetes, and hypertension. Let’s dig into the science behind sleep and what are our five best tips for a good night’s rest!
Why sleep is so important to our bodies
Sleep gives your body some much-needed rest, but it’s also vital for maintaining your cognitive health. When you lie down to sleep at night, your body takes this time to cleanse your brain of toxins and waste. The space between your brain cells actually enlarges during sleep, allowing your body to wash out harmful substances like beta-amyloid proteins, which researchers have linked to the formation of Alzheimer’s disease. It follows, then, getting enough sleep can help ward off Alzheimer’s disease.
A poor night’s sleep has also been tied to forgetfulness and lapses in memory. Because sleep is the vital period when our brains take time to consolidate our memories, not getting adequate sleep makes you more likely to forget things during the day. A good night’s rest is one of the most powerful weapons in your arsenal in the fight against mental aging.
Why getting enough rest is more difficult as we age
Production of the “sleep hormone” melatonin naturally decreases with age, making it harder for older adults to fall asleep and stay asleep. The aging process also causes changes to the body’s natural circadian rhythm, which can make you get tired earlier than usual. Because of this, older adults are also more likely to experience restless sleep and waking up throughout the night.
Environmental factors can also be to blame, such as stress or a lack of structure in your life. Recent retirees sometimes have a hard time adjusting to changes in their schedule, which can lead to fitful sleep.
How to get a good night’s sleep: build healthier sleep habits
Now that you know why a good night’s sleep is so vital, you’re probably wondering how you can improve the quality of your own rest. If you struggle with tossing and turning or restless nights, don’t worry. The good news is that healthy sleep habits are universal and can be practiced by anyone of any age.
It’s never too late to establish a healthy nighttime routine! Here are our 5 best tips to help you combat insomnia, in no particular order.
Work up a sweat

Exercise helps to keep you in good shape, but did you know that exercising can also improve your sleep? The Sleep Foundation has demonstrated a clear link between exercise and improved sleep quality in adults. Try using a fitness tracker, which can be useful to show your progress and motivate you.
To rest easier at night, try going for a brisk walk or bike ride outside. Exposing yourself to sunshine and fresh air can improve circadian rhythm, so you can stay active with your favorite outdoor hobbies like gardening and fishing. Just be careful not to exercise too late in the day–getting worked up too close to bedtime may actually keep you awake!
Don’t nap during the day
Napping is common among older adults and retirees, with research showing that around 25% of older adults take naps daily. But did you know that your daily power nap may actually be doing more harm than good?
It’s true. While a brief nap can be beneficial for a boost of energy, excessive napping can disrupt your circadian rhythm and make it harder to fall asleep at night. If you absolutely must have a nap, try to take it earlier in the day and make sure to sleep for no more than 30 minutes.
Establish a bedtime routine
Human beings are creatures of habit, so practicing good habits before bed can help improve your rest. If you don’t already have one in place, try establishing a nightly routine before drifting off to sleep.
You can engage in soothing activities like taking a bath, reading a book or meditating, to relax before bed. Sleep comes easier in a cold room, so make sure that your bedroom is cool before you lie down. Always try to fall asleep at roughly the same time every night to establish routine, and make sure that you fall asleep while lying in bed–not in a recliner or on the couch.
Turn off the TV
Although many of us like to fall asleep with the glow of the TV to keep us company, staring at screens before bed can actually disrupt your sleep. The blue lights found in common electronic devices like smartphones, tablets, TVs and computers can disrupt your natural circadian rhythm. That’s why experts recommend cutting out all screens and electronic devices before going to bed.
A few hours before your usual bedtime, turn off all your TVs and power down your tablets, phones and laptops. You can replace time in front of the TV with screen-free activities like doing a jigsaw puzzle, playing cards or drawing in an adult coloring book. Instead of sleeping with your phone on your bedside table, try plugging it up to charge in another room. You’ll be less likely to check for texts or emails in the middle of the night and can rest more peacefully.
Cut back on caffeine and other foods
Eating or drinking certain things too close to bed can cause sleep problems. Foods high in caffeine like coffee and chocolate have been shown to disrupt sleep patterns and interfere with melatonin production. Drinking alcohol late at night also could lead to restless sleep because it can cause decreased REM sleep. Never use alcohol as a sleep aid.
If you can’t do without your morning coffee, that’s perfectly all right. Just make sure that it stays a morning cup. Avoid consuming coffee in the afternoon and eating large meals too close to bedtime. Don’t drink too much water before bed, either, if waking to go to the bathroom is a problem for you. If you must eat before bed, try having something to boost your melatonin, like a handful of almonds or a cup of tart cherry juice.
The bottom line
Along with diet and exercise, getting a good night’s sleep is one of the most important things you can do to maintain a healthy mind and body.
If you’ve tried all these tips and nothing works,
contact Aviv Clinic and schedule a free consultation with our care team: click here
Exercise and Brain Health: Tips to get the most from your workout
The science is pretty clear: exercising and maintaining good health are some of the best things you can do to keep the body at peak performance. But there are more than a few options out there when it comes to exercising. Exercise and brain health are closely linked. Are some forms of exercising better than others when it comes to the brain? Are there right–or wrong–ways to exercise when it comes to maximizing brain power? And how does exercise affect the aging brain?
Aviv Clinics clients receiving the innovative hyperbaric oxygen therapy treatment optimize their brain health because their personalized treatment plan combines cognitive and physical training, plus receive nutritional coaching. As part of the program, clients exercise on the cutting-edge h/p/cosmos medical treadmill at the clinic. The combination of physical and cognitive effort maximizes the benefits of the treatment protocol.
How cognitive abilities change with age
While most Americans fear losing their memory and cognitive abilities, far fewer actually do. As we get older, a slight level of cognitive decline is inevitable due to the normal aging process. It’s common to have issues with memory and slower thinking. But older adults are also increasingly at risk for mild cognitive impairment and dementia, the latter of which includes conditions like Alzheimer’s disease.
While some of the risk factors for these conditions are out of your control, such as age, genetics, and family history, your overall health plays a role, too. Staying healthy and active can protect the brain.
Lifestyle matters

Our brains haven’t changed much in the last 50,000 years or so, but our lifestyle certainly has. In the days of our nomadic, hunter-gatherer ancestors, life was a little more physically demanding–our bodies are designed to move and be active. Sitting, it seems, could be making us sick.
According to LifeSpanFitness, these days the average American sits for 11 hours a day, and an estimated 20% of all deaths over age 35 can be attributed to a sedentary lifestyle. Lack of exercise, poor diet, and use of alcohol, tobacco, or drugs are often a starting point. Falling into this sedentary lifestyle can quickly lead to a downward spiral.
The spiral of decline
If there are underlying conditions or you have risk factors for certain conditions, a sedentary lifestyle can exacerbate them or lead to chronic disease. Dealing with chronic illnesses is difficult even with access to good healthcare, but many do not or cannot get proper care, further exacerbating present conditions. Helplessness and hopelessness about the situation can then lead to anxiety and/or depression. You may feel like you can’t live the life you used to, and may find yourself self-isolating. Unfortunately, declining physical and mental health can set you up to be even less active, and the cycle continues.
Your brain isn’t the only organ affected by this vicious cycle; this kind of lifestyle can lead to problems with cardiovascular health as well. In fact, they seem to be intricately linked; in general, things that improve heart health improve brain health, too.
How are exercise and brain health linked?
Anytime that you exercise, you’re pumping more blood to your brain tissues, and with that comes a lot of oxygen and other nutrients, vital for the brain’s functioning. In response, the brain also cranks out some helpful molecules. Here are just a few benefits of exercise for the brain:
-
- Neurotransmitters (NTs) like serotonin, norepinephrine, and dopamine are released, improving mood,
motivation, focus, attention, and learning - Brain-derived neurotrophic factor (BDNF) helps your brain repair and rebuild, creating new neurons and
connections - Hormones work with BDNF and can boost your mood and mental clarity
- Endorphins and other molecules are released, helping relieve pain
- Increased blood flow delivers nutrients and carries away waste products
- The hippocampus increases in volume
- Neurotransmitters (NTs) like serotonin, norepinephrine, and dopamine are released, improving mood,
Two areas of the brain are particularly important when it comes to cognitive decline. The prefrontal cortex (PFC) and the hippocampus. These areas are the most susceptible to cognitive degeneration or impairment.
The hippocampus, which is responsible for memory and learning, is affected by exercise in a few ways. Studies have shown that aerobic exercise can actually increase the volume of brain matter in the hippocampus, an area that will often decline in volume as we age and significantly with Alzheimer’s disease. It’s also where a lot of neurogenesis (creating new brain cells) is going on–at least if you’re exercising enough!
The other area that benefits directly from exercise is the prefrontal cortex–this is the CEO of the brain, responsible for most of our executive functions including decision making, attention, problem-solving, and goal setting. Studies have shown that older adults in particular can benefit from exercise due to increased executive functioning.
What’s the best kind of exercise?
Getting oxygen-rich blood pumping to the brain seems to be the best way to reap the benefits of exercise. Therefore, aerobic exercise (or cardio) is a good place to start. While all types of exercise have benefits, most of the studies favor those that elevate your heart rate and keep it there for a time.
The “prescription” for most older adults is to aim to exercise at a moderate-intensity for 30-45 minutes, 3-4 times per week. An easy way to keep track of your progress is with a fitness tracker. Find out if they are right for you.
Moderate intensity can be measured by keeping your heart going at the optimal rate, in this case, 70-80% of your maximum heart rate. To find out your max heart rate, subtract your age from 220. For example, a 70-year-old’s maximum heart rate would be 150. That means that to exercise at the right intensity, she should maintain a heart rate between 105-120.
You should warm up and cool down for aerobic exercise, but don’t count that as part of your total. The 30-45 minutes (as prescribed) should all be while your heart rate is at the target rate.
Tips for getting started
If you’re like many (if not most) adults, you might be starting more towards the sedentary end of the activity scale. The exercise prescription above is an ideal goal, and it’s used primarily because that’s what they did in the studies that showed the best outcomes for cognitive health. However, other studies showed that lower-intensity activities like walking (5 miles a week) and yoga could be beneficial, too.
Even if you’re aiming for that peak exercise intensity, there are lots of ways to make exercising for brain health more fun, easier, and less stressful.
Find movement that you love

Exercise is about movement, so find a way to move your body that you enjoy. If that’s running laps, great. If you love to dance, then dance! And there’s always sports and leisure–gardening, golfing, bowling, are all ways to move. Even window shopping or hula hooping can count as exercise. Need more ideas? Try any of these non-boring exercises!
Finding movement you enjoy can also help change your perspective and shift away from goals like weight loss that may feel like a chore. Focus on the way exercise makes you feel and the enjoyment you get from moving.
Start from where you are
If you’re already pretty active, or you’ve exercised a lot in the past, it’ll probably be easier for you to start. If you are not as active as you could be, that’s okay! It’s never too late to begin a new exercise practice.
If you really want to get the benefits of brain-boosting exercise, be aware of where you’re starting from and build from there. If you’re sedentary, jumping into an intense workout routine could be difficult physically and frustrating mentally. You’re more likely to stick with it if you’re realistic about your goals and abilities.
Focus on frequency
If you’ve struggled in the past to start an exercise practice, you’re not alone. Exercising consistently means forming a new habit, and that’s no easy feat. Starting any habit takes time, effort, and consistency for a little while. But the awesome benefits of habits are that once they’re formed, they’re automatic.
It might be tempting to jump in at full duration and/or intensity, but it’s also a good way to burn out. In the beginning, it helps to focus more on when and how often you exercise rather than how hard or how long. Even a few minutes a day is enough to tell the brain “this is what we do now.” Eventually, you won’t have to remind (or force) yourself to exercise anymore. Once the habit is formed, it’s much easier to increase the intensity and duration.
Add it up
Ultimately, it’s about moving more and being more active. There are many ways to sneak in more exercise and break up the sitting. For example, if you do sit a lot, you can try setting a timer to get up and walk around every hour. Or start counting your steps and aim to increase them every day.
Many of the classic ways to get more activity are still great, like taking the stairs, parking farther away, playing with kids, or housework and cleaning. Make it a goal to find a new way to squeeze in some activity every day.
Be patient
So how long does it take before exercising starts to pay off? While many of the benefits of exercise can be felt immediately afterward, such as improvements in mood and energy, lasting results will take longer. Plan on giving it at least six months to assess your brain’s progress.
When it comes to cognitive abilities, measuring and assessing can be a challenge. You may not notice a substantial increase in cognitive ability. As some cognitive decline will occur due to normal aging, it’s often about slowing it down rather than a full reversal. It’s also common for family and friends to notice a change before you do.
The bottom line on exercise and brain health
Find movement that you enjoy, and you’ll have a much easier time making time to exercise. No matter what shape you’re in or what activities you enjoy, you can find a way to optimize both your physical and your cognitive health.
PTSD and Traumatic Brain Injury: What’s the link?
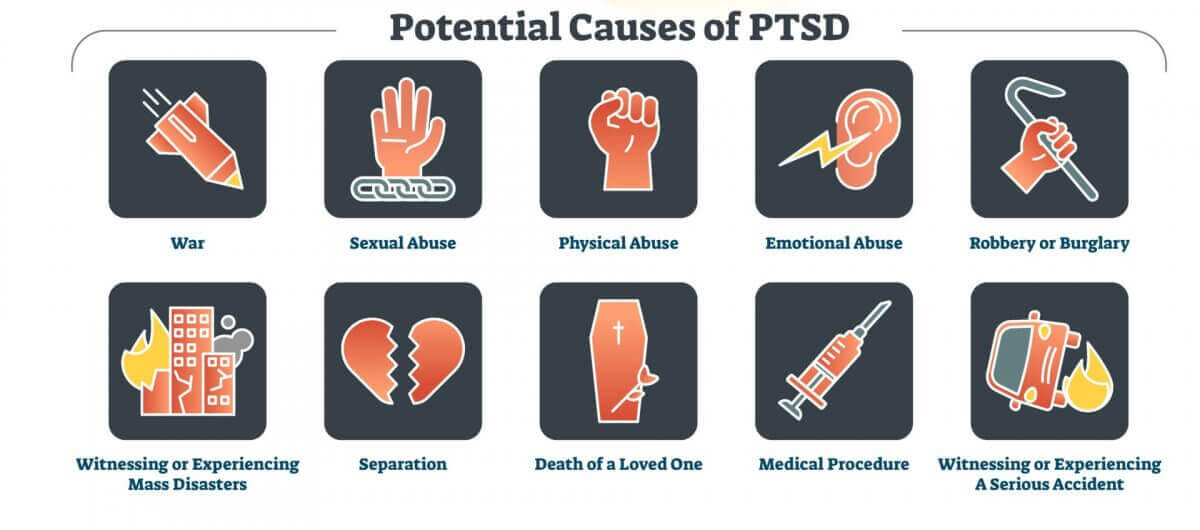
War veterans probably spring to mind when most people think of post traumatic stress disorder (PTSD). But many kinds of traumatic events can cause people to develop PTSD.
About 60-75% of Americans will experience at least one traumatic event during their lifetime, and the majority will experience more than one. Events could include natural disasters, life-threatening accidents, physical or sexual assault, the sudden death of a loved one, or the diagnosis of a serious illness; even simply witnessing such events can be traumatic.
Not everyone who goes through a traumatic event will develop PTSD. Most people will process the trauma and move on. However, twenty percent will develop PTSD.
PTSD may take months or even years to develop. It can potentially affect your physical, mental, emotional, and cognitive health in a number of ways, including:
- Intrusive symptoms such as memories, flashbacks, or nightmares
- Avoidance of people, places, etc. that trigger memories of the event
- Negative changes in thinking patterns and mood
- Emotional changes, including heightened emotions or conversely feeling numb
- Heightened arousal and reactivity
- Cognitive impairments such as memory, attention, or concentration struggles
- Sleeping problems and insomnia
The full list of symptoms can be found here.
PTSD can develop after physical trauma, such as an accident or natural disaster, or due to psychological trauma alone, such as seeing someone die or being mugged at gunpoint.
PTSD and Traumatic Brain Injury
PTSD shares a considerable amount of overlap with traumatic brain injury (TBI), and researchers are trying to figure out why. Not only are the two conditions difficult for clinicians to distinguish between, but they also frequently occur together.
A large study of US Army soldiers who fought in Operation Iraqi Freedom reported that 43.9% of the soldiers who had TBI with loss of consciousness also met diagnostic criteria for PTSD. Another study reported that having a TBI doubled the chance of developing PTSD.
Traumatic brain injuries are generally caused by a blow to the head, injuries that pierce the skull and brain, or things such as whiplash that can cause the brain to bump into the skull. Like PTSD, TBI is not limited to combat vets; every year, at least 1.5 million people in the US experience a TBI.
Depending on the severity, TBI can be mild, moderate, or severe. It’s even possible to have a TBI and not even know it! Mild TBIs (mTBI), also known as concussion, can involve the following symptoms.
- Headache
- Dizziness
- Nausea
- Fatigue or drowsiness
- Speech problems
- Sensory issues such as a bad taste in the mouth
- Sensitivity to light or sound
For moderate TBIs, the symptoms above can be more severe and also accompanied by the loss of consciousness.
Most people with mild and even moderate TBI recover within days to months. However, about 15% will show symptoms of post-concussive syndrome a year later. The symptoms include most of the same ones that could have immediately followed the trauma. But it could also include persistent emotional challenges such as mood lability, anxiety and/or depression, and cognitive impairments like mental slowness or memory or concentration issues, like brain fog.
Interestingly, those who have a mild TBI are more likely to develop PTSD than those with more severe brain injuries. The likely reason is that those who experience a more violent blow to the head tend to have amnesia around the traumatic event, ironically sparing them from the flashbacks, nightmares, bad memories, and more that are often caused by PTSD.
What’s the connection?

The same traumatic event can cause TBI, PTSD, or both, especially if the traumatic event involved psychological as well as physical trauma, such as war combat or domestic violence.
One condition can also affect the course of the other. For example, PTSD that develops following a car accident could complicate recovery from brain injuries sustained; conversely, a TBI may block the person’s ability to get emotional closure from the psychological aspects of the event.
How do they cause cognitive issues?
Until recently, researchers didn’t understand exactly what these conditions were doing in the brain, and in particular how they affected cognition.
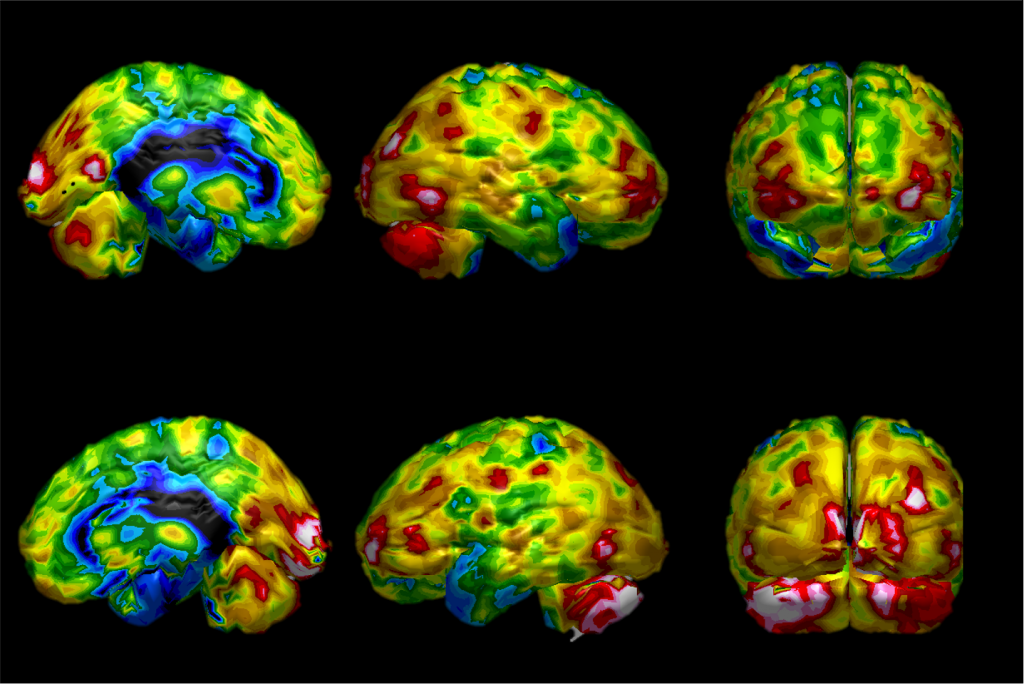
According to this review, TBI and PTSD represent “brain disorders with disruptions in neural networks that communicate via long axonal pathways through white matter tracts, termed the “connectome.” The connectome is the brain’s “wiring” pattern; the sum total of billions of neurons and the pathways or routes that they use to carry out their function.
Both TBI and PTSD have shown to produce neural inflammation, excitotoxicity, and oxidative stress within the brain. These processes, all of which can affect one another, represent normal functions in the body that, under every day conditions, don’t cause harm. If these functions get pressed into service too often or for too long though, they can kick into overdrive and quickly spiral out of control, leading to cellular damage and physical changes in the brain.
For example, the amygdala is largely responsible for the “raw data” of emotions that arise in the body. But it’s your prefrontal cortex that actually works with the amygdala to regulate emotions. Studies have shown that a critical connection between the prefrontal cortex and amygdala may be broken in brains with TBI or PTSD, which could explain the commonly seen lack of emotional control.
The bottom line
PTSD and TBI can both be debilitating conditions that greatly affect everyday life for those who suffer from them. However, recent research into the neural mechanisms of these disorders has opened the door for the discovery of new treatment options.
How Does Sugar Affect the Brain?
From the Paleo diet to the Mediterranean diet to the ketogenic diet and beyond, there’s one thing that nearly all modern diets agree on—if you want to maintain a healthy body and mind, cut out sugar.
While there’s wisdom in this advice, blanket statements like “cut out sugar” can leave room for confusion. It leaves many people wondering, is all sugar bad for you? Should you avoid sugar in any form, including in fruits? What about carbohydrates found in vegetables like potatoes? With so many complicated questions like these and no clear answers, it’s no wonder many people feel confused. As a center dedicated to improving brain health and performance, Aviv Clinics understands the importance of proper nutrition and its direct effect on cognitive and physical functioning.
Let’s examine sugar in detail and clarify what dietitians really mean when they tell you to cut out sugar.
Is Sugar Really the Enemy?
Not exactly—foods with high amounts of sugar can still be healthy! For example:
- Apples contain lots of sugar but water, vitamins, nutrients, and dietary fibers that are vital for a healthy body. Dietary fiber is essential for maintaining a thriving wealth of gut flora. Gut flora builds our immune system and fights off ailments like leaky gut disease.
- You can find natural sugars in many whole foods. They also come in many different chemical forms, including glucose from carbohydrates. Glucose provides our bodies with energy, helping fuel our muscles and vital organs as it circulates throughout the bloodstream. We wouldn’t be able to function normally without the glucose from carbohydrates.
Does Your Brain Need Sugar?
Although the brain can use alternative fuel sources for fuel if you’re insulin resistant, such as ketones, glucose is the brain’s preferred fuel source. The brain relies heavily on glucose when performing complex tasks requiring much thought.
So when you’re concentrating extra hard on a crossword puzzle or a complicated passage in your favorite book, your brain is burning glucose over time to help you get the job done. If your blood sugar dips too low, you can experience problems like brain fog or trouble concentrating. It’s your brain’s way of telling you that it needs more fuel and that you should grab a healthy snack.

What Is the Difference between Natural Sugar and Refined Sugar?
While natural sugar naturally occurs in foods, refined sugar is processed to extract the sugar.
Natural Sugar Process
When you eat an apple, your body does all the work of processing the unrefined fruit into digestible nutrients all on its own.
First, you must chew the apple, breaking it down into apple sauce. Then, your gut does the hard work of absorbing the vital nutrients and breaking down the sugar to send circulating throughout your bloodstream.
The leftover fiber is used to nourish your gut’s network of microflora. When you eat whole foods, your body is the factory, and the natural sugars in your foods are the fuel that runs it.
Refined Sugar Process
Foods with refined sugar are a different story. Candies, cookies, chips, and other pre-packaged snacks don’t offer your body the same fuel as whole foods. Your body doesn’t have to go through the work of breaking down these highly processed foods—the factory already did it for you.
Processed foods are loaded with refined sugar without any of the nutrients, vitamins, and fibers your body needs. This leaves your gut flora starved of the materials required to function and your immune system vulnerable.
Is Sugar Bad for Your Brain?
It’s possible to have too much of a good thing. Modern western diets are filled with refined sugar and carbohydrates in the form of ready-made snacks, treats, and processed foods.
Thus, you may feel sluggish once the “sugar high” wears off. Eating too much sugar can also make you susceptible to health conditions like type 2 diabetes.
The best way to limit refined sugar intake is to lean on a natural diet consisting of whole foods.
What Does Sugar Do to Your Brain?
Excessive sugar intake can impact specific neurotransmitters and bring on memory deficiencies. Among these neurotransmitters is dopamine—the chemical controlling mood, behavior, learning, and memory.
Here’s what research studies further illustrate:
- When rats were fed a high-sugar diet that resembles the average western diet, their cognitive performance suffered. The rats struggled to complete tasks that relied on their memory. Their struggles suggest their diets were directly responsible for impairing their brain’s prefrontal lobe and hippocampus regions.
- Eating a diet high in sugar can reduce the production of a chemical called “brain-derived neurotrophic factor” (BDNF). This chemical is active in areas of the brain vital to learning, memory, and higher thinking. Low BDNF levels are associated with poor memory function and are linked with Alzheimer’s Disease and dementia.
- Experiments in animals and people have revealed that when the brain needs an extra power boost, blood vessels in the brain dilate to deliver more glucose and oxygen through the bloodstream.
Is Sugar Important to the Body?
Yes, natural sugars in the foods you eat perform a vital role in energizing the body and mind. The body requires a total of 200 grams of sugar or glucose each day. Two-thirds of this, or 130 grams, is used by the brain to help you function to your best ability.
The key takeaway from the information we presented above is this—incorporating a diet filled with natural, whole foods is essential to:
- Nourishing your body with the right type of sugar
- Enhancing cognitive and physical performance
4 Tips for Healthy Eating
The natural sugars found in whole foods are nothing to fear. Eating a diet with enough carbohydrates and natural sugars is vital for keeping your body and brain healthy.
Here are a few ways to stay on track:
- Make sure the bulk of the sugar you consume comes from whole foods like fruits and vegetables, not processed junk foods.
- Just because a food is labeled “sugar-free,” that’s not always the case. It may be true that a food doesn’t contain added sugar, but remember that carbohydrates turn to glucose in your body.
- You can rack up carbohydrates quickly on a typical day. Try to aim for around 45 total carbs at every meal if you’re a woman or 60 every meal if you’re a man. You’ll be surprised how quickly you can meet that quota with just a handful of whole foods!
- You don’t have to cut out refined sugar altogether. Obsessing over eating a “perfect” diet only stresses you out and doesn’t leave any room for you to feed your soul. Do you plan on spending a relaxing afternoon baking with your grandkids? Go ahead and treat yourself to a warm cookie fresh from the oven.
If you’re eating healthy at most meals, there’s no need to feel guilty about indulging in rich foods now and then. Just be smart about it, and always make conscious decisions about what kind of foods you put into your body.
Aviv Clinics delivers a highly effective, science-based treatment protocol to enhance brain performance and improve the cognitive and physical symptoms of conditions such as traumatic brain injuries, fibromyalgia, Lyme, and dementia. The Aviv Medical Program’s intensive treatment protocol uses Hyperbaric Oxygen Therapy and includes nutrition management and dietitian support to optimize your diet for better brain health. Based on over a decade of research and development, the Aviv Medical Program is holistic and customized to your needs.
Contact us to learn more.
Cognitive Impairment & COVID-19: What We Know So Far
There’s a lot that we still don’t know about COVID 19, especially when it comes to the long-term effects. However, emerging research suggests a troubling new link between the Coronavirus and long-term neurological dysfunction. Many “COVID long-haulers” continue to experience headaches, dizziness, fatigue, and brain fog even weeks after recovering from the Coronavirus. Research also suggests links between the virus and increased risk for strokes, which is concerning for older adults or anyone who already had an increased risk.
If you’ve been feeling lost and dazed since recovering from the Coronavirus, you’re not alone. But don’t despair. In this article, we’ll address the potential neurological effects of COVID-19, along with our best advice for COVID long-haulers.
What is a “COVID long-hauler”?
“COVID long-hauler” is a new term used to describe the growing number of people who continue to experience symptoms of the Coronavirus weeks after recovering. Common complaints among long-haulers include respiratory problems like a persistent cough or shortness of breath. Neurological problems are also common, including headaches, fatigue, loss of taste/smell, and the now-infamous “Covid brain fog”.
Long-haulers are a diverse group, and anyone can become one, young or old. It’s not unusual for someone to report feeling like they’re “in a fog” or “stuck in a daze” even weeks after testing negative for the virus. Some people may be plagued by COVID fatigue or headaches, while still others can’t taste their favorite foods.
You don’t need to have been hospitalized to be a COVID long-hauler, either. Even mild cases can lead to these unpleasant after-effects, which is why you still don’t feel like your old self even after a minor bout with the virus. It’s unclear exactly why some people become COVID long-haulers while others experience no ill effects. But researchers are working hard to gain a greater understanding of the risk factors involved.
How COVID affects the brain
Did you know that when it comes to COVID, losing your sense of smell is actually a neurological problem? It’s true. The Coronavirus can affect the olfactory nerve connecting your nose to your brain, which inhibits your sense of smell. It was one of the earliest signs that COVID could affect the brain. While we still need more research to determine the full extent of COVID’s neurological effects, preliminary studies have revealed a connection between the virus and impaired cognitive performance.
In the study, a group of COVID-19 patients between the ages of 30 and 60 underwent a series of neuropsychological tests to assess various functions of their brains, including memory function, processing speed, and executive function. The COVID-19 patients experienced inhibited cognitive function when compared to a healthy test group, and they especially struggled with sustaining attention on the tests, providing us with evidence that the “COVID brain fog” is a real phenomenon.
Further studies have also provided us with links between COVID and headaches and COVID and strokes, giving us a greater understanding of how the virus can impact the brain.
The inflammation connection
Interestingly, COVID patients also exhibit high levels of inflammation in their blood. That’s not surprising since inflammation is one of the immune system’s natural responses to threats. In low levels, inflammation is a good thing; it’s a sign that your body is addressing the problem as intended. But as with everything in life, balance is key, and excessive inflammation can wreak havoc on your health.
One of the symptoms associated with coronavirus is a “cytokine storm”, an overactive immune response that skyrockets inflammation levels. Cytokine storms have been associated with reduced oxygen in the blood and other respiratory problems caused by COVID-19. They’ve also been linked to neurological problems, like brain fog, fatigue, or the stabbing headaches associated with the virus.
COVID and Strokes
While it’s still unclear exactly why COVID increases the risk of ischemic strokes (blood clots) in some people, inflammation could play a part. Chronic inflammation has long been linked to an increased risk of stroke, which could explain why the aging population is more susceptible.
Picture two highways. One highway is smooth and freshly paved without any potholes or blemishes. It’s easy for traffic to flow through this highway on a consistent basis, and traffic jams are uncommon. On the other hand, the second highway is littered with potholes, cracks, and closed lanes, all of which make it difficult for traffic to flow even on a good day. Now, which highway do you think will fare better when a snowstorm strikes?
The highways in this analogy are your blood vessels, and the flow of traffic is your blood cells. The snowstorm is, of course, COVID-19. Having high levels of inflammation in your body makes it easier for the blood to clot, which can ultimately lead to strokes. This is also why those with pre-existing conditions are hit hard by the virus — because their immune systems are already inflamed from fighting other problems.
How to combat inflammation
Because COVID patients almost always exhibit higher levels of inflammation in their blood, having low inflammation levels in your body can help combat the severity of the virus. Eating a clean diet, exercising regularly, getting plenty of sleep, and avoiding stress keeps inflammation levels low, which can help COVID long-haulers find relief. Avoiding stress is especially key, although that’s often easier said than done.
If you’re feeling stressed because of the pandemic, you’re definitely not alone. If the constant barrage of information from the news and social media is stressing you out, try unplugging for a while. Fire up the iPad for a chat with your grandkids, or head outside for a (socially-distanced) walk in the fresh air. While it’s important to stay informed, it’s also important to take care of your mental health.
Could getting vaccinated help a COVID long-hauler?
What about the Coronavirus vaccine? If you’re a COVID long-hauler plagued by brain fog or headaches, could getting vaccinated provide relief? Unfortunately, probably not. The purpose of the vaccine is to train your body’s immune system to fight against the Coronavirus. It’s meant to be used as a preventative measure. It’s not a cure, and it’s not a way to mitigate the virus’s after-effects. That’s no reason not to get vaccinated, however.
Even if you’ve already contracted the virus, the vaccine can prevent you from getting it a second time, which can minimize your risk of suffering long-term side effects. And if you’ve never contracted the virus before, getting vaccinated can ensure that you never have to deal with long-term side effects in the first place.

When to see a doctor about your long-term Coronavirus symptoms
If you’re struggling with long-term COVID neurological symptoms, you don’t need to suffer alone. Whether you’re being plagued by fatigue, brain fog, dizziness, headaches or loss of taste, any problem that impacts your quality of life is worth bringing up to your doctor.
Although your doctor may not have all the answers yet, they’ll do everything they can to help you cope with your symptoms. There’s also the possibility that your symptoms may not be caused by COVID at all, but by another health condition instead. Never hesitate to seek help when you need it, especially when it comes to your cognitive well-being.
The bottom line
While we still need more research to determine the full extent of the Coronavirus — especially when it comes to long-term symptoms — anyone of any age can minimize the damage caused by COVID simply by practicing healthy lifestyle habits and keeping your inflammation levels low. Taking care of your body inside and out is crucial not just for fighting COVID, but for any health condition you may encounter.
You can also minimize your chances of contracting the virus by continuing to follow the CDC guidelines of mask-wearing, social distancing, and getting vaccinated when you can. Above all else, staying calm and optimistic is one of the most important things you can do in the face of the pandemic. So do your best to stay positive.
Telomeres and Reverse Aging: A Deep Dive into the Connection
Aging seems to be an inescapable part of life: spines shrink, skin wrinkles, and attention spans dissipate. But what if aging was escapable—or at least reversible? What if scientists were able to target the root cause of aging in our very own cells and treat it as if it were an illness?
Researchers in Israel have conducted the world’s first study to prove that biological aging can be reversed:
- Scientists were able to reverse the biological aging process in “thirty-five healthy independently living adults, aged 64 and older.” Through the targeted application of a unique hyperbaric oxygen therapy (HBOT) protocol.
- Telomeres are one of the critical biomarkers of age, and they naturally shorten during the aging process. The research study showed HBOT may help with “increasing telomere length…in the aging populations.”
- These findings are truly groundbreaking, given the accessibility of hyperbaric oxygen treatment. However, Aviv Clinics in central Florida is the only center in the United States to offer this unique HBOT treatment protocol.
So how did these researchers manage to accomplish such a seemingly impossible task that existed only in science fiction just 50 years ago? The answer lies in telomeres—a critical component of your DNA.
What Are Telomeres?
A telomere is a protective cap found at the end of each DNA strand in the human body. They are considered one of “two key hallmarks of the aging process.”
The two types of age to keep in mind are:
- Chronological age, or how many birthdays you have had
- Biological age, or the age that reflects your body’s functions
When considering telomeres, here’s how they manifest in age:
- Short telomeres equate to an older biological age.
- Longer telomeres equate to a healthier, younger biological age.
So it is entirely within reason for a healthy 60-year-old (chronological age) to be much younger (biologically speaking) if they have long, healthy telomeres to continue to protect their cells.
Telomeres and Shoelaces
Telomeres work much like the hardened end caps of shoelaces. Those components on your shoelaces protect the delicate strings they are connected to. Without a protective cap, a shoelace can quickly become frayed and unusable.
As long as the cap persists, a shoelace can stay intact for quite some time. Similarly, telomeres prevent damage from occurring to your underlying DNA:
- With intact telomeres, your cells are protected and they can continue functioning like normal.
- Without telomeres, your cells essentially begin to age and die.
Telomeres and DNA
DNA is a commonly understood component of human biology. Few people go through life consciously thinking about how DNA functions.
Let’s change that with some facts:
- Your DNA contains the biological instructions necessary for your body to continue developing.
- Millions upon millions of cellular processes occur within a human body at any given time.
DNA manages those processes, calmly instructing your cells to divide, consume, and produce complex proteins to stay alive. Telomeres play a vital role in this function.
Telomere Length Naturally Decreases with Age
As we age chronologically, our telomeres naturally shorten. This exposes our DNA, leaving our bodies vulnerable to the diseases and effects of aging.
Some of the common diseases of aging—onset by shortened telomeres—include:
- Heart disease
- Stroke
- Diabetes
- Cancer
- Dementia
When the telomeres in your cells become too short, they enter an aged, unhealthy state called senescence. In senescence, a cell can no longer divide to continue replenishing the body’s vital tissues, which makes a person more susceptible to the diseases listed above.
Stress May Impact Telomere Length
External factors like stress can also affect telomere length. The American Psychological Association (APA) reports:
- “Chronic stress and cortisol exposure decrease your supply” of telomerase—the enzyme that replenishes telomeres. So when stress affects your life heavily, you become more susceptible to shorter telomeres.
- Stress is now “one of the most consistent predictors of shorter telomere length.” Exposure to life hardships (e.g., childhood neglect or caregiving in late adulthood) has been particularly noted for its impact on telomere length.
How Aging Manifests
Keep in mind, aging can look different for everyone. Some individuals may notice physical or cognitive changes as they age.
Physical changes may include:
- Wrinkled or sagging skin
- Whitening or graying hair
- Immune, metabolic, kidney, or liver issues
Cognitive changes may include:
- Memory trouble
- Mood shifts
- Slower executive function (e.g., thinking and decision-making, multitasking)
What Is Reverse Aging?
Now for some good news: Whatever type of aging you face, reversing it is possible. When referring to “reverse aging,” we mean biological age. Though chronological aging is inevitable, certain treatments can manage some of the biological shifts that occur because of natural aging and external factors.
The Research Behind Telomeres and Hyperbaric Oxygen Therapy (HBOT)
With the importance of telomeres and aging now understood, most people ultimately want to know:
- How to protect their telomeres, and
- How to repair any degradation that has already occurred.
The scientific research team led by Dr. Shai Efrati, founder and director of the renowned Sagol Center for Hyperbaric Medicine and Research in Israel, proved—for the first time—that reversing biological aging is possible.
By using hyperbaric oxygen therapy (HBOT), Dr. Efrati and his team of scientists were able to increase the length of telomeres in people aged 65 or older by more than 20%.
Research Method
HBOT involves the patient inhaling pure oxygen in a pressurized environment. This study was conducted on 35 different adults aged 65 and higher. Patients had their blood measured before the study, as well as during the 30th and 60th sessions of HBOT.
Research Findings
The findings were truly unbelievable:
- The telomere length of patients who received HBOT “increased significantly by over 20% following HBOT”—in just three months!
- “There was a significant decrease in the number of senescent [cells],” reducing the number of these dangerous, aging cells with little-to-no telomere length by as much as 37%.
These findings were the basis for creating the cutting-edge HBOT protocol only available at Aviv Clinics.
How Can I Protect My Telomeres?
“Telomere length is genetically determined, with heritability estimates ranging from 44% to 80%.” Fortunately, that still leaves you with a wide margin to protect!
Thankfully, there are many different ways you can protect your existing telomeres and thus control damage and the negative impacts of aging. These include:
1. Exercise Regularly
Research has shown that people with high levels of physical activity have significantly longer telomeres than moderately active or sedentary adults. More specifically, adults who regularly exercise demonstrate a biological age difference of nine years when compared to those who don’t.
2. Maintain a Balanced Diet
Like regular exercise, a balanced diet is crucial in protecting telomere length. High levels of body fat create high levels of oxidative stress—stress that directly affects your cellular integrity.
To protect the length of your telomeres, you must reduce the levels of oxidative stress in your body. Maintaining a healthy, balanced diet rich in antioxidants can provide your DNA with the proper protection it needs to maintain healthy, long telomeres.
3. Avoid Smoking & Alcohol Use
You already know that smoking and drinking alcohol aren’t the healthiest decisions—but did you know that people who smoke have shorter telomeres than those who don’t?
Likewise, people who excessively consume alcohol experience faster levels of biological aging than those who don’t. The science is in: If you’re interested in protecting the length of your telomeres, stay away from tobacco and alcohol.
4. Manage Stress
Stress, especially higher cortisol levels, is one of the main reasons for shortened telomeres. Stress takes many forms, but we are mainly concerned with psychological, chronic, and life-related stress.
These kinds of stress raise the levels of oxidative stress placed on the cells of your immune system. Fortunately, there are many wonderful methods for mitigating stress in our daily lives. Whether it is mindfulness, martial arts, or meditation, you will likely be able to find a method that works best for you.
Fight Aging with Aviv Clinics
Aging manifests differently for everyone, but help is available. Aviv Clinic’s age-related decline program is based on research and has helped many clients restore the youthful vitality they seek and deserve.
If you’d like to learn more about how you can boost your cognitive or physical performance while reversing the effects of aging, contact our team.
Could I have a Traumatic Brain Injury and Not Know It?
As the years go by, many of us chalk up lapses in memory as a side effect of aging. But if you’re also experiencing headaches, trouble concentrating, and thinking clearly, then something more serious may be to blame: a traumatic brain injury. What, a brain injury? Surprisingly, yes. Brain injuries are more common than most people realize, and left unchecked they can wreak serious havoc in your life. Fortunately, the latest scientific advancements, such as hyperbaric oxygen treatment protocol, show promise in helping treat traumatic brain injuries.
According to the Brain Injury Association, more than 2.8 million people sustain a traumatic brain injury (TBI) every year, and TBI-related deaths are highest among older adults. Since symptoms of a traumatic brain injury can sometimes take years to manifest, many people don’t even realize that they have one until problems show up later in life. That’s right: the fall you had in the 1990s could actually be the cause of your headaches and brain fog today.
TBIs can cause all sorts of cognitive problems and can even lead to permanent disabilities if left unchecked. You don’t even need to directly hit your head to obtain one, either. But the good news is that with proper detection, traumatic brain injuries can be treated, including at centers such as Aviv Clinics. That’s why we’ve put together this helpful guide with everything you need to know about TBIs and how to determine if you may have one.
What is a Traumatic Brain Injury?
A traumatic brain injury (TBI) is exactly what it sounds like. It’s a form of brain injury that occurs when an external trauma is inflicted upon the brain. This trauma can impair your brain’s ability to communicate with the rest of your body, and the effects can differ depending on the part of your brain that was injured. Damage can range from mild to severe and there is not always a loss of consciousness.
The most common form of a mild TBI is a concussion, which is caused by a violent shaking or rattling of the brain. Common causes for TBIs include: Sports injuries, Falling off a bike or horse, Military injuries, Being assaulted or struck, Being in a car accident, Falling and hitting your head.
Any kind of scenario involving your brain hitting your skull can cause a TBI, such as whiplash from a car accident. Although the potential for sustaining damage is greater if you were knocked unconscious, you don’t have to lose consciousness to experience negative effects. Even mild brain injuries can cause symptoms to appear in the long term.
TBI symptoms checklist
What are the symptoms of a traumatic brain injury? Just like the severity of a TBI can vary, so too can the severity of the symptoms you experience.
Signs of a concussion or mild TBI include:
– Headaches and dizziness
– Nausea and vomiting
– Changes in sleep patterns
– Confusion or Memory Loss
– Fatigue or lethargy
– Difficulty concentrating
– Difficulty making decisions
– Mood changes like depression or irritability
Although many people feel the effects immediately after sustaining a brain injury, symptoms can show up at any time, even years later. This delay means that many people never make the connection between hitting their head and cognitive problems experienced later in life.
In some cases, a TBI may never be properly diagnosed because the person who sustained it never lost consciousness or never went to the doctor afterward. Many people suffer needlessly because they never realize they sustained a TBI to begin with, and the effects of an untreated TBI can be devastating.
TBIs can even lead to more sensory problems like blurred vision, ringing in the ears (tinnitus), or even difficulty understanding language and communicating properly (aphasia). And because TBIs and dementia can have similar symptoms, it’s important to know what you’re dealing with so that you can receive the proper treatment.
How do you detect a TBI?
There are different ways to evaluate for a TBI. Brain injuries can cause two distinct types of damage: structural and metabolic. Structural damage is caused by physical damage to the brain, such as bleeding. Metabolic damage affects the brain cells themselves. A CAT scan or MRI is the first step to detecting obvious structural damage in the brain. But there can be more subtle damage to your brain that these scans might miss, especially if your injury is years old. This is where more advanced techniques come into play.
Functional MRIs or SPECT scans can detect metabolic damage in the brain tissue.
These scans can reveal improperly functioning brain cells even years after the bleeding has stopped.
From there, your healthcare provider can move forward with treatment options.
SPECT scan – enables doctors analyze the metabolic activity of portions of the brain
How do you treat a TBI?
One of the most promising treatments for brain injuries involves hyperbaric oxygen therapy (HBOT).
HBOT is a treatment where patients receive oxygen-enriched air in a special high-pressure chamber. The unique hyperbaric protocols were researched and tested for years at the Sagol Center for Hyperbaric Medicine and Research in Israel. They are now available at the Aviv Clinic, Jumeirah Lakes Towers (JLT), Dubai, U.A.E
HBOT has been shown to improve neuroplasticity and lead to the improvement of chronic impairments in patients with mild TBIs, even on brain injuries that are years old. HBOT also induces angiogenesis in the brain, the process by which new blood vessels form from existing ones. These structural changes in the brain can lead to improvements in thinking clarity, cognitive performance and overall quality of life!

Hyperbaric Suite, Aviv Clinics, Dubai.
Conclusion
While the name may sound scary, TBIs are both detectable and treatable, even years after they occur.
With the proper care, you can see improvements to your memory, cognitive function and overall quality of life!
For more information about Aviv Clinic’s personalized program and unique hyperbaric protocol, or to schedule an in person consultation, contact the clinic today.
The Effect of Intermittent Fasting on Your Brain
There’s a lot of debate in the health and wellness sphere about the best diet for your health. Where some swear by low-carb high-fat diets, others insist that high-carb low-fat is the only way to eat. With so many conflicting opinions, it’s difficult to know whom to trust or what to listen to. Fortunately, there is a way you can eat that may help you lose weight, improve your brain health, and even increase your longevity, all without strict dietary restrictions. Best of all, it’s not a “diet” at all!
This “non-diet” is intermittent fasting, which is quickly building up steam in the dietary community. Unlike fad diets, fasting is more than just a passing trend because it’s as old as humanity itself. Our bodies are designed to fast, and you already do it every day. From the time you eat your last meal at night, to the time you eat breakfast in the morning, you’re fasting. Intermittent fasting is about gradually pushing out this window until your brain and body start reaping the benefits.
As a center dedicated to improving brain health and performance, Aviv Clinics understands the importance of proper nutrition and its direct effect on cognitive and physical functioning. Making dietary changes, such as Intermittent fasting, benefits brain health, promotes weight loss, and prevents certain diseases. Here’s more on intermittent fasting, along with how you can start fasting yourself.

What is Intermittent Fasting?
Intermittent fasting is an eating style that involves alternating between periods of eating and fasting.
Intermittent fasting is not a diet; it’s a lifestyle. You’re in charge of your own meal plan, and you can customize it to your liking. You can combine intermittent fasting with the Mediterranean diet, Paleo, Keto, DASH, or any other diets. If you don’t want to follow a particular diet, just make sure that you make healthy food choices. Try to avoid artificial ingredients or overly processed foods. So long as you meet all your nutritional requirements within your eating window, just about anything goes!
Because you’re not tied down by the restrictions of a traditional diet, you have the freedom to customize your meals to your own preferences. This means that you’re more likely to stick to a consistent diet plan, which is essential if you want to lose weight and keep it off.
Is intermittent fasting healthy?
Although conventional advice would have us believe that we need to eat every 2-3 hours to sustain ourselves, our evolutionary history paints a different picture. Our hunting and gathering ancestors didn’t have regular access to food like we do, so their bodies had to develop a way to operate without a consistent source of glucose. That’s where fasting comes in as a survival mechanism.
In the same way that you might clean your home and throw out the things you don’t need, fasting is our body’s way of cleaning up shop. Fasting for extended periods allows your body to cleanse itself and use up leftover nutrients from the previous day’s meals, which triggers a process called “metabolic switching”.
Metabolic switching slows the aging and disease processes and promotes weight loss in obese individuals. Fasting also prevents breast cancer in both women and men, and studies suggest that it may improve longevity. Eating constantly doesn’t allow the body time to properly rest, which means you won’t experience the cleansing benefits of metabolic switching.
What fasting does to the brain?
Intermittent fasting is amazing for maintaining brain health. In addition to slowing the aging process, metabolic switching increases neuroplasticity in the brain. This helps optimize brain function and increase the brain’s resistance to injury and disease. Intermittent fasting also triggers a process called autophagy, which works to ward off Alzheimer’s disease and Parkinson’s.
Fasting can also clear brain fog and sharpen the mind. Many people who fast report clearer thinking and improved moods, which can benefit your brain-gut connection and increase your overall happiness.
Intermittent Fasting for Beginners
There are a few different ways to practice intermittent fasting.
Some of the most common methods include:
Time-restricted fasting
This is the most common method of fasting, and the one most people will end up practicing. It works by limiting the daily window where you eat your food every day. For example, if you eat your first meal of the day at 10 am and your last meal at 6 pm, then you’ve fasted for 16 hours and eaten for 8, meaning that you followed a 16:8 fasting schedule. Common ratios for time-restricted fasting include 14:10, 16:8, 18:6 and 20:4.
5:2 Fasting
This method of fasting involves eating normally for 5 days a week and fasting for two. On fast days, you’ll eat one 500 calorie meal if you’re a woman, or one 600 calorie meal if you’re a man.
Alternate Day Fasting
This is a more extreme version of 5:2 fasting. Instead of fasting for only two days a week, you’ll fast on alternating days, following the same 500-600 plan for meals on fast days.
Start with time-restricted fasting before trying the more advanced options. Just like you can’t expect to run a marathon without experience, you can’t expect to fast for hours on end without a little training first.
Try gradually shrinking your eating window every day until you’ve reached your goal. If you currently eat your first meal at 8:00 am, try pushing it out to 9:00 am and eventually to 10:00 am or 11:00 am. Or if you want to try 5:2 fasting, start out by fasting only one day a week and gradually upping it to two. Whatever fasting schedule you choose, just try to be consistent. Establishing a routine and sticking to it helps establish consistency, which is key for a healthy lifestyle.
What constitutes breaking a fast?
If you’re interested in giving fasting a try, you might be wondering about what counts as breaking a fast.
Will your morning cup of coffee ruin your fasting schedule or not? The answer is, it depends.
While calorie-free beverages like coffee or tea are all right to drink while fasting, anything that has calories in it breaks a fast. That includes any kind of artificial sweeteners or creamers you may add to your favorite drink.
That doesn’t mean that you have to drink black coffee exclusively, however. You can make a game out of adding creamer to your coffee at a later time every day. Try challenging your family members or friends to see who can hold out with black coffee the longest!
Is there anyone who shouldn’t fast?
People with Type 1 diabetes or anyone who takes insulin shouldn’t fast. This can put you at risk for dangerous blood sugar problems like hypoglycemia or ketoacidosis. People with hypertension, blood pressure problems, or cognitive impairments shouldn’t fast either, and neither should anyone who struggles with remembering to eat on a daily basis.
Certain medications may also prevent people from fasting, and those who use canes or wheelchairs should also take care not to fast. As with any diet, check with your healthcare provider if you’re not sure that fasting is right for you.
Conclusion
The benefits of intermittent fasting are numerous and clear. It can increase your lifespan, lower your risks for diseases and improve your brain’s overall health. But perhaps fasting’s biggest benefit is that it allows you to put the joy back in eating. When you don’t have to worry about weighing, counting or measuring, you can focus on eating foods that nourish not only your body, but also your soul.
You can still indulge in your family’s traditional recipes without feeling guilty. It’s important to eat a balance of foods that make you happy and foods that keep you healthy. Intermittent fasting provides you with the perfect framework for this, allowing you to live your best life possible exactly the way you want to.
DP World’s Aviv Clinics Dubai
Nutrition is an important pillar in your approach to health, especially as you age. The Aviv Medical Program utilizes a multidisciplinary approach to healthy aging, including a personalized nutrition plan based on a comprehensive assessment to address your individual needs and goals, along with hyperbaric oxygen therapy, physical training, and cognitive training.
Discover how you can take your brain health and longevity into your own hands with Aviv Clinics. Learn more today.
Meditation and Brain Health: Benefits Backed by Science
The COVID-19 virus has left us all more stressed than ever before, but there’s one group of people that the pandemic has hit especially hard: older adults. A recent poll conducted by the National Poll on Healthy Aging interviewed 2,000 adults from the ages of 50 to 80. More than half (56%) of the participants reported struggling with feelings of isolation during the pandemic, a dramatic increase from 27% in the 2018 poll.
Long hours spent indoors away from family and friends can have us all feeling low, and the stress and loneliness can wreak havoc on your mental health. That’s why many older adults are turning to the practice of mindfulness meditation to cope with stressful feelings during the pandemic.
Just like washing your hands to get rid of germs, meditation is an excellent way to help cleanse your mind of troublesome thoughts, and practicing mindfulness can do more than just help you relax. Taking a few minutes out of your day to ground yourself in the present moment is one of the most rewarding things you can do for your mental health, and the benefits are backed by science.
The science-based Aviv Medical Program is centered on the innovative hyperbaric oxygen therapy, cognitive and physical training, plus nutrition coaching. Supportive wellness practices, such as meditation, help to create a truly holistic approach to enhancing cognitive and physical performance.

What is meditation? The art of mindfulness
Mindfulness meditation is the art of being present in the here and now.
It’s about taking a few minutes every day to clear your mind of distressing thoughts and engaging with what’s right in front of you.
Think of it as a workout for your brain. In the same way that you might lift weights to keep your body strong, meditation is a way to train your mind and increase your focus and awareness. It’s not a spiritual practice or a mystical art; it’s a learned skill and anyone can learn to meditate, regardless of age.
5 Benefits of meditation backed by science
There are several proven benefits to meditating regularly. Numerous studies have shown that mindfulness practices like meditation and yoga can improve all sorts of mental health problems. From easing anxiety and depression to stalling memory loss in Alzheimer’s patients, here are our top 5 benefits of meditation.
1. Slows the progression of Alzheimer’s disease
Although many people dismiss lapses in memory recall as a side effect of growing older, there’s no scientific evidence to suggest memory loss is a natural side-effect of aging. On the contrary, forgetting valuable memories doesn’t have to be the new normal for older adults.
Meditation has been proven to improve memory recall in adults in as little as eight weeks. Research also shows promising results in the use of mindfulness to slow the progression of cognitive conditions like Alzheimer’s disease and dementia. Patients who practiced mindfulness exercises reported reductions in cognitive decline and stress levels, and overall improvements to their quality of life.
Mindfulness isn’t only beneficial for those diagnosed with cognitive conditions, either. Studies have also shown that caregivers of those with cognitive impairments can benefit from the stress reduction of practicing meditation. In other words, everyone can benefit from the boost to cognitive centers of the brain.
2. Improves focus and keeps your brain sharp
Practicing mindfulness can keep your brain active and in good shape, no matter how good your memory is. You don’t have to be a seasoned expert. Even beginners can reap the benefits of mindfulness meditation.
In one study, participants who listened to a 10-minute meditation tape experienced increased attention spans and focus when completing a test compared to those who didn’t meditate beforehand. One researcher further confirmed that people who meditate regularly consistently perform better on focus-related tasks. The same study also found that meditation calms the areas of the brain associated with mind-wandering and spontaneous thoughts, helping you stay focused on what you are doing in the present.
3. Combats insomnia
Getting a good night’s rest is more important than ever for seniors and older adults. Sleep is the vital period when our minds cleanse themselves of harmful waste. Yet current research estimates 10-30% of people are affected by chronic insomnia, with older adults showing more susceptibility to sleep disturbances.
A randomized trial found that mindfulness meditation significantly improved sleep quality in middle-aged and older adults. The lowered stress levels provided by meditation helps clear your mind from troubling thoughts, which can make sleep come easier. If you have trouble sleeping at night, turn off your screens and try meditating for a few minutes before bed.
4. Fights anxiety
Although everyone worries from time to time, harboring too much stress in your body can be unhealthy. According to researchers, anywhere from 3-14% of all older adults meet the diagnostic criteria for generalized anxiety disorder. Unchecked anxiety and stress can worsen health conditions like fibromyalgia and lead to other mental health problems like depression.
If you want to take control of your anxious thoughts, meditation may be the solution. Studies have shown that mindfulness meditation can alleviate symptoms of generalized anxiety disorder and reduce stress levels, helping you clear your mind of fears and worries.
5. Improves depression and overall mood
Loneliness was already a common problem among older adults and retirees, but the COVID-19 pandemic has made it worse. Going out in public and visiting your family isn’t an option for many older adults, and the isolation can worsen feelings of loneliness and despair
Practicing mindfulness can help you manage these difficult emotions and improve your overall mood. Studies have shown that mindfulness training reduces feelings of loneliness and isolation, helping participants be happier in the present moment.
Mindfulness training has been shown to help reduce feelings of depression in adults. Those who practiced meditation therapy reported fewer symptoms of depression compared to their counterparts who didn’t meditate at all. Practicing mindfulness every day reminds you not to stress over every little thing, helping you stay calmer and more in control of your emotions.
How to start a mindfulness meditation practice
You don’t need any special equipment or training to get started. All you need is a comfortable place to sit and the willingness to give it a try. Here’s a quick guide to get you started:
1. Find a quiet space where you can relax, free from distractions.
If you’re inside, make sure that all televisions and electronic devices are turned off.
2. Sit in a comfortable position and breathe gently.
3. Pay attention to each inhale and exhale.
4. Focus on all the sensations of your body as you breathe.
5. Release any tensions you may be holding until you are completely relaxed.
6. Continue to breathe in and out as you focus on your body’s inner sensations.
7. If your mind wanders, that’s ok. Just re-focus on your breathing and start again.
8. Keep going for 5-10 minutes or as long as you’d like to meditate.
Try to meditate at the same time every day to establish a routine. If you don’t want to sit in silence, you can find guided sessions via apps on your smart devices, or you can play some calming music to help you focus. For added benefits, try meditating outside on the porch or in a garden. Doing your daily session in nature can calm you even further, helping you make the most of your mindfulness practice.
The bottom line
Mindfulness meditation is one of the most positive things you can do for your mental health and emotional well-being. It doesn’t take long to do, either. Having a simple routine to keep your mind in-shape can show benefits across all areas of your life. From improving memory recall to lowering stress levels and improving your sleep, practicing meditation can keep you more engaged in the present moment, helping you stay happy and calm during the best years of your life.
Aviv Clinics delivers a highly effective, science-based treatment protocol to enhance brain performance and improve symptoms of conditions such as traumatic brain injuries, fibromyalgia, Lyme, and dementia. The Aviv Medical Program’s intensive treatment protocol uses hyperbaric oxygen therapy and takes a holistic approach that includes brain training to achieve optimal results. Based on over a decade of research and development, the Aviv Medical Program is customized to your needs.