6 Future Trends in Healthcare for Patients
As healthcare rapidly evolves, patients must keep abreast of these shifts. Doing so activates your role in driving better health outcomes for yourself and your loved ones.
COVID-19 showed how technology can benefit patients during the pandemic. The medical community in Dubai is leveraging those takeaways to elevate patient care.
Additionally, individuals want to take more ownership of their health through the convenience of personalized, educational, and digital care.
Look out for these six future trends in healthcare throughout 2023 as more healthcare providers take steps to meet patient needs.
1. Remote Patient Monitoring (RPM)
COVID-19 showed how critical technology could benefit patients and elevate care. One way to achieve this has been through remote patient monitoring (RPM).
In 2022, RPM tools (e.g., wearable devices, pulse oximeters, blood glucose meters, and heart monitors) were valued at $53.6 billion. This value is projected to reach “USD 175.2 billion by 2027.”
When “74% of all deaths globally” are attributed to at least one chronic disease, a physician’s ability to remotely manage health conditions is key to preventing hospitalizations—remote patient monitoring (RPM) can reduce “the number of ER visits and hospitalizations.”

2. Health Literacy
With more doctors and patients remotely managing conditions, healthcare organizations are providing digital platforms that offer personalized educational experiences—experiences that address each patient’s health literacy level (in their preferred language and reading level).
As more providers anticipate higher patient volume (from individuals who delayed or avoided medical care during the pandemic and from the return of medical tourism), you’ll see more educational materials at each touchpoint of your care journey.
Don’t hesitate to discuss literacy levels with your doctor to ensure you feel confident and comfortable navigating your health journey.
3. Mindfulness Products
Wellness has taken center stage since 2020, with mindfulness coming to the forefront as an in-demand component:
- McKinsey reports “mindfulness has gained mainstream consumer acceptance relatively recently” among patients. Half of the survey respondents expressed that they wish more mindfulness products and services were available.
- Medical research indicates mindfulnesses exercises such as meditation can reduce “cognitive decline” and “perceived stress.”
Don’t be surprised to see more providers offering holistic care. For example, healthcare organizations may consider partnering with mindfulness apps or providing products that offer mental health benefits.
4. Data Analytics
Objective data is critical to seeing how you’re progressing and what additional steps you and your physician need to take.
More doctors are tracking and sharing with their patients the data that reports:
- Interaction with educational materials
- Treatment and communication gaps that need addressing for better outcomes
- Patient progress along a personalized treatment plan
- Actionable steps a patient takes to manage their health (remotely or in-clinic)
Data transparency helps the provider and the patient understand how a condition is progressing and what can be done to elevate treatment.
5. Advanced Imaging
The development of new technologies has brought on better ways to treat patients. One prime example is advanced imaging and neuroscience.
Advancements in radiography give medical professionals the tools to perform in-depth assessments of the brain upon a stroke. Advanced imaging may include:
- 3T MRI with DTI (diffusion tensor imaging)
- SPECT scan with new AI analysis methods
These imaging technologies help providers map a personalized recovery plan and track recovery in post-treatment assessments.
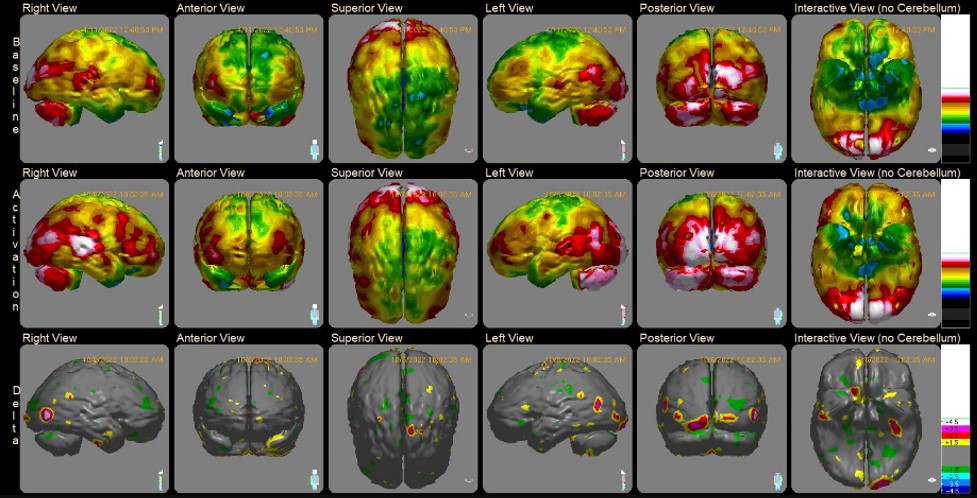
Comprehensive medical programs, such as the one at the Aviv Medical Program, rely on these advanced imaging and neuroscience tools to earn long-term results for stroke patients.
6. Hyperbaric Oxygen Therapy (HBOT)
Oxygen is the lifeblood of our health. As we age, body oxygen levels decrease, leading to infamous age-related decline. While most of these shifts are often thought to be irreversible, research says otherwise.

Studies indicate hyperbaric oxygen therapy (HBOT) can help:
- “Reverse biological aging” by slowing down the growth of cells and protein structures responsible for the aging process.
- “Reverse the main activators of Alzheimer’s disease”
At Aviv Clinics, our unique HBOT program entails fluctuating oxygen levels, which triggers the body’s self-regeneration capabilities.
“By treating vascular dysfunction, we’re mapping out the path toward Alzheimer’s prevention. More research is underway to further demonstrate how HBOT can improve cognitive function and become an influential tool in the imperative fight against the disease.” -Dr. Shai Efrati, Aviv Clinics
Learn More about Hyperbaric Oxygen Therapy
Aviv Clinics Dubai, brought to you by DP World, is here to elevate your healthcare journey, offering the world’s most advanced Hyperbaric Oxygen Program.
Our diverse community of patients has achieved significant health milestones thanks to a multidisciplinary approach that can include:
- In-depth review of health history
- Comprehensive physical exam
- Highly advanced MRI, DTI, and SPECT scans
- Neurological and neurocognitive tests
- Body composition analysis
- Cellular performance analysis
- A detailed report of our assessment findings
- Unique Hyperbaric oxygen therapy (HBOT) protocol
- Cognitive training
- Physical training
- Dietary coaching
- A post-treatment report of your improvements and recommendations for future progress
Our unique medical approach centers on research to provide high-quality care that produces lasting improvements in mental and physical performance. Areas of improvements include:
- Memory
- Concentration
- Information Processing Speed
- Emotional Health
- Stamina
- Energy
- Mobility
- Independence
- Quality of Life
- Sexual Performance (Men)
- Sleep
Benefits of our program also include:
- Stem cells proliferation– the building blocks of tissue rejuvenation – to multiply and migrate
- Lengthen the telomeres – the protective caps at the end of each strand of DNA
- Reduce senescent cells – known to contribute to many age-related diseases
- Increase mitochondrial function – the power plant in each of our cells
If you’ve experienced cognitive or physical decline due to aging or disease, we may be able to help.
To learn more about the Aviv Medical Program, contact the Aviv Clinic.
Life After a Diagnosis of Cognitive Decline: What Now?
Whether you have received a diagnosis of mild cognitive decline, dementia, or Alzheimer’s disease, exploring the possible causes is the first step in moving forward.
Symptoms like forgetting where you have placed your glasses, frequently asking the same question, or failing to recognize familiar people may have led you to seek medical attention. Perhaps your family noticed changes in your mood or personality and urged you to see a doctor. Being evaluated and having a diagnosis may be initially disconcerting and stressful, but how you proceed from here will determine your best outcome.
Often, what may be causing the cognitive issues is something controllable and treatable such as high blood pressure, high blood sugars, stress, anxiety, medications, or drug and alcohol use. No matter what is behind the decline, the key is addressing those things that can be controlled and treated, and then choosing a healthier lifestyle going forward.
What is cognitive decline?
Cognitive impairment is when a person has trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life. It can range from mild to severe, escalating to the point where the person loses the ability to comprehend, write, or speak. At that stage, a person can no longer live independently.
Age is the greatest risk factor for cognitive impairment.
According to the Centers for Disease Control and Prevention (CDC), more than 16 million people in the United States are living with cognitive impairment. An estimated 5.1 million Americans aged 65 and older currently have Alzheimer’s disease, the most well-known form of cognitive impairment; this number may rise to 13.2 million by 2050, the CDC reports.
Next steps
Stress and anxiety will most certainly follow on the heels of a diagnosis. Learning to cope in healthy ways will be crucial because stress and anxiety can worsen symptoms of cognitive decline. You may be tempted to isolate because you fear being embarrassed by your condition or want to hide your frustration when you are challenged to remember. However, do not shy away from being challenged. Do just the opposite.
Interact even more and engage in things that bring you joy. How you proceed after diagnosis could slow the progression or alter the trajectory of the disease.
Here are six things to do immediately no matter the diagnosis:
- Eat a healthy balanced diet with plenty of fruit and vegetables, good proteins and healthy fats, and limit those foods that contain saturated fats like butter and cheese. Some examples of brain-beneficial foods include coffee, blueberries, nuts, dark chocolate, and fatty fish like salmon, tuna, and sardines. Fatty fish contain omega-3 fatty acids which the brain uses to build brain and nerve cells, and are essential for learning new things and storing memories.
- Exercise for at least 30 minutes, five times a week. Whenever you exercise, you are pumping more blood to your brain tissues, and with that comes a lot of oxygen and other nutrients vital for the brain’s functioning. Walking or swimming are great ways to get oxygen-rich blood pumping to the brain.
- Challenge your brain daily with activities that keep it stimulated like doing puzzles, taking quizzes, and reading content you enjoy. They help exercise the brain, enhance creativity, improve problem solving, and may slow memory decline.
- Get adequate sleep. Stay away from things that may overstimulate your body like tea or coffee before bedtime. Put down your phone or computer a couple of hours before bedtime so you can decompress naturally and slowly. Sleep allows your body to cleanse the brain of toxins and waste. Getting enough is essential.
- Find a good support system. It will be critical to build a good support system now that you have received a diagnosis. Whether it is a spouse, a friend, a family member, or a support group, having a connection with someone who cares about you and knows what you’re going through can keep you from feeling alone.
- Manage stress. Self-medicating with drugs and alcohol will only worsen the symptoms of cognitive decline. Instead, try journaling, prayer, meditation, exercise, or whatever works to calm your inner spirit and reduce your stress load.
The prognosis
In some people, mild cognitive impairment can be reversed or remain stable, especially if it is linked to a medication. For others with a diagnosis of dementia or Alzheimer’s disease, the outlook can be harder to swallow since both are progressive conditions, and symptoms will eventually worsen. However, making lifestyle changes like healthy eating and exercising may slow the rate of progression.
The bottom line
Maintaining healthy lifestyle choices, including proper nutrition, exercise, social and cognitive activities, and adequate sleep, may help prevent or delay cognitive decline. For those who receive a diagnosis, the best approach moving forward is to cherish every moment of clarity, enjoy every day you are gifted, and maintain as many healthy choices as possible to slow down the disease.