Emotional Problems after a Traumatic Brain Injury in Children and Youth
Children and youth have so much to learn and experience—areas that are key for future health and development. Because their brains are still growing, it’s essential to protect and nurture their physical and cognitive health. But as life goes, accidents happen. Children sometimes forget to wear their helmets or buckle their seatbelts. And conditions like a traumatic brain injury (TBI) can suddenly change the course of their life.
Traumatic Brain Injury (TBI) can have devastating effects on individuals of all ages, but children and youth are particularly vulnerable due to the crucial brain development that occurs during this time.
Because of brain maturation, the consequences of TBI evolve as a child grows. In some instances, brain plasticity (the ability of the brain to learn and adapt) may help to regain skills or compensate; but in many instances, the true implications of TBI may not be apparent until the child is older.
In addition to physical and cognitive impairments, children and youth who suffer TBI often experience psychological and emotional problems that can have a significant impact on their quality of life. The symptoms will vary depending on the area and extent of injury to the brain. Some of the most common psychological changes, outlined below, can manifest days or weeks after the accident and can persist long after the initial injury.

Emotional problems commonly associated with TBI in children and youth:
Learning how a TBI affects mental health is an important step to improving your child’s emotional and behavioral health.
5 Emotional Problems Associated with a TBI in children:
- Depression: Children with TBI may experience feelings of sadness, hopelessness, and a loss of interest in activities they once enjoyed. Sadness is a normal response to experiencing an accident. But when these feelings become chronic, your child may be dealing with depression. Depression can be particularly challenging for children and youth as it can impact their ability to concentrate and learn in school.
- Anxiety: Children with TBI may experience excessive worry or fear, which can interfere with their ability to participate in activities and social situations.
- Irritability and mood swings: Children with TBI may experience sudden and intense changes in mood, including irritability, anger, and frustration. In some cases, children with TBI may become aggressive and display behaviors such as hitting, kicking, and biting. These mood swings can be challenging for both the child and their caregivers to manage.
- Attention-deficit/hyperactivity disorder (ADHD): Some manifestations of ADHD include disruption in the classroom, the inability to focus, or having trouble understanding and completing schoolwork. Children with TBI carry “an increase in risk for ADHD.” As many as “one in five kids” who have a TBI develop ADHD.
- PTSD: Children who have experienced a traumatic incident can also develop post-traumatic stress disorder (PTSD). Symptoms may include nightmares, sleep problems, and/or reliving the event in their thoughts.
It is important to note that the severity and duration of these emotional problems after a TBI can vary greatly depending on the individual child and the extent of their injury.
Traumatic Brain Injuries (TBI) in children are a significant public health concern in the United Arab Emirates (UAE). According to a study published in the Journal of Neurotrauma, where motor vehicle accidents and falls were the leading causes of TBI in children, accounting for 70% of cases.
Learn more about emotional problems after a traumatic brain injury and how hyperbaric treatments have shown promise in “improving brain function and quality of life.”.

Misdiagnosis of Emotional Problems after a TBI in Children
For children with a TBI, the emotional and behavioral symptoms they experience are often incorrectly diagnosed as other conditions. This misdiagnosis can lead to the wrong treatment or cause delays in recovery. A misdiagnosis can have serious consequences, as it can lead to inappropriate treatment and delay in addressing the underlying TBI.
For example, treating a child with TBI with medication for ADHD may not effectively address the underlying brain injury and may even worsen symptoms. It is therefore important for healthcare providers to consider the possibility of TBI when evaluating a child’s emotional and behavioral symptoms, especially if the child has a history of head injury.
Traumatic brain injury is often referred to as a “hidden” disability, because some of the effects appear small but they may have a great effect on function. Accurate diagnosis is critical for providing appropriate treatment and support for the child’s recovery. Caregivers and family members should also advocate for their child’s needs and ensure that they receive a comprehensive evaluation that includes consideration of a potential TBI.
Seek Help for Your Child with a Holistic Assessment and Rehabilitation Plan
Cognitive and emotional problems after a traumatic brain injury may be treatable. The key is to find a medical team who offers a personalized assessment and treatment plan. Such a plan may include a combination of the following protocols:
- A comprehensive assessment of your child’s cognitive, behavioral and physical performance, including advanced anatomical and functional brain scanning.
- Hyperbaric oxygen therapy (HBOT)
- Cognitive training
- Physical training
A Unique Hyperbaric Oxygen Protocol to Improve Youth Traumatic Brain Injury
At Aviv Clinics, we have a unique approach to treating TBI and its effects on our youth patients.
We offer a comprehensive program that is backed by over a decade of scientific research, that employs hyperbaric oxygen therapy (HBOT) in addition to an individualized cognitive and physical rehabilitation program.
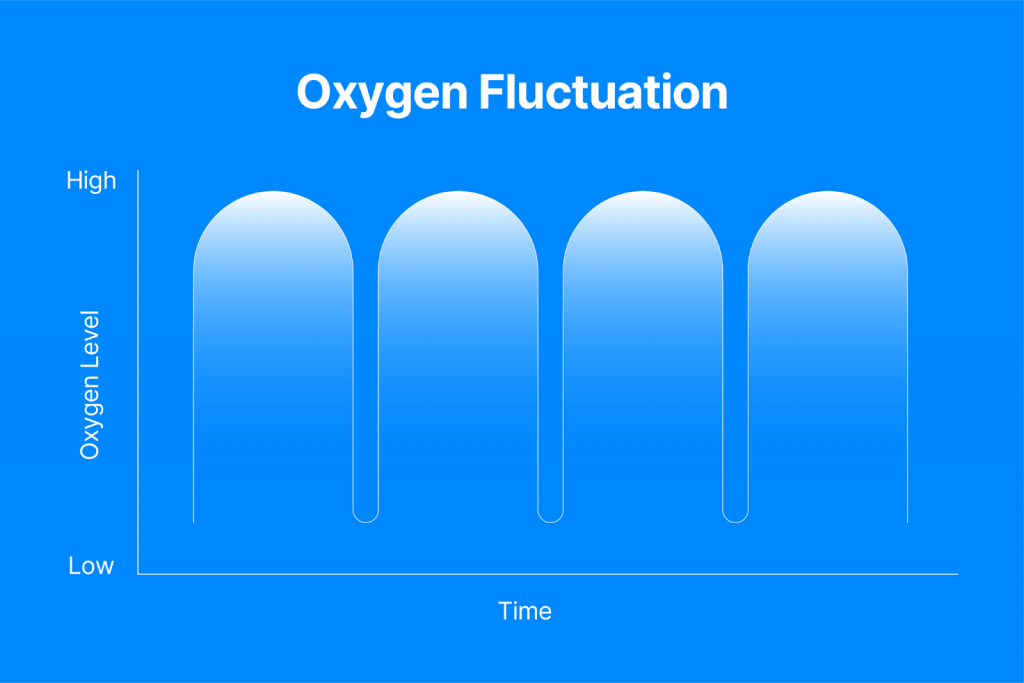
The Aviv Hyperbaric treatment is offered inside our state-of-the-art, luxurious hyperbaric suite, where the young patient sits and breathes 100% oxygen through a facemask, at a pressure of 1.5 ATA (ideal for children and youth), and includes a unique hyperbaric protocol that triggers the self-regenerative mechanism of the brain and body.
A recent study published in Nature Scientific Reports, shows the effectiveness of Hyperbaric treatment in healing damaged brain tissue and alleviating symptoms in children experiencing persistent post-concussion syndrome (PPCS), where concussion symptoms continue beyond the expected recovery period.
The study suggests that HBOT improves cognitive and behavioral function, as well as quality of life in pediatric patients suffering from PPCS, even years after their traumatic injury.
Learn more about – Hyperbaric Oxygen Therapy for TBI
TBI Survivor Story: Linden Perry – Watch her story
At just 15 years old, Linden dealt with multiple concussions from soccer. These accidents left her with post-concussion syndrome (PCS), which caused debilitating physical and cognitive issues. Time went on with no real improvements. Her traumatic brain injury left her frustrated and unable to perform as well as she wanted to in school and sports.
Linden and her mother, Clarissa, sought a customized and diverse treatment plan at Aviv Clinics that included the following:
- Hyperbaric oxygen therapy
- Cognitive training
- Physical training
After completing the treatment, Linden could finally go to both study and sports. More importantly, she feels more like herself. The long-term health complications she once faced no longer impact her ability to participate in activities.
Clarissa says, “[Linden] seems happier and more like the Linden before.”
Learn More about TBI Treatment in Dubai
If your child has not been the same since their accident, our team of medical professionals can lend a hand. The Aviv team is here to help improve the quality of life for your loved one.
Watch the video about our unique approach:
Can Concussion Symptoms Be Delayed?
The mind and body are complex. We might think we know what is happening inside our bodies, but sometimes it’s not very obvious.
According to estimates, “69 million individuals are estimated to suffer TBI from all causes each year.” Experiencing post-concussion syndrome symptoms years later is not uncommon. If you’ve endured a motorbike or car accident, the brain injury that occurs can manifest on its own timeline.
Fortunately, recovery from delayed symptoms is possible even years after a traumatic brain injury. The Aviv medical team is here to explain why concussion symptoms can be delayed and what you can do to treat them. Use this guide to regain control of your health—the foundation of a good life.
Delayed Symptoms of Concussion: Why They Happen
For some people, concussion symptoms will come on immediately. Others have symptoms that come and go. And yet some people exhibit symptoms only later in life.
For example, a patient with a concussion might initially have headaches that resolve quickly. Then over time, these minor headaches develop into new and debilitating symptoms (e.g., chronic and/or more severe headaches).
Delayed symptoms from a concussion may include physical and mental effects, such as:
- Headaches
- Nausea or vomiting
- Balance problems or dizziness
- Blurred vision
- Sensitivity to light/noise
- Memory or concentration problems
- Depression and/or anxiety
- Mood swings
What to Do If You Suspect You Might Have Delayed Symptoms of Concussion?
Rest assured, there are several clinically and scientifically proved treatments for post-concussion syndrome. They include:
- Physical therapy (PT): Aims to ease pain and improve mobility and range of motion of different joints. This includes different types of manual therapy, exercises, and a range of other modalities.
- Cognitive behavioral therapy (CBT): Psychological treatment that strives to change thinking and behavioral patterns
- Hyperbaric oxygen therapy (HBOT): Involves breathing 100% pure oxygen in a room known as an HBOT suite to increase oxygen levels in the body up to 20 times higher than average to improve cognitive, physical, and psychological performance
Read more about the common post-concussion syndrome (PCS) treatment options.
How Does the Brain Recover from a Concussion?
The brain is a powerful organ with self-healing mechanisms. The key is finding the right treatment program to give the brain the delicate push it needs to unleash its potential.
The right medical expertise and protocol can help:
- Encourage neuroplasticity, or the brain’s ability to adapt and react in response to injury or disease
- Drive neurogenesis, or nerve cell regeneration that occurs in the brain
- Increase blood flow and oxygen in the parts of the brain associated with executive function, vision, sensation, and other responses
How Long Does It Take To Recover?
Most patients at Aviv see progress within about 8-12 weeks of the start of their treatment plan. But the recovery period varies depending on the condition’s severity and the patient’s health background, lifestyle, and other factors.
The best treatment plan will offer lasting results. Even if you have post-concussion symptoms years after an accident, there is still hope for recovery.
Aviv Clinic’s Unique Hyperbaric Oxygen Therapy (HBOT) Protocol
At Aviv Clinics Dubai brought to you by DP World, our team proudly executes a highly-advanced HBOT and rehabilitation program backed by research and data. We take a holistic approach to healing. Our unique HBOT protocol involves specific, personalized fluctuations of oxygen levels in the suite to kick-start the body’s recovery process.
“Hyperbaric oxygen therapy can be successful because it addresses the cause of the symptoms, not just the symptoms alone. In combination with cognitive, physical, and nutritional coaching, some HBOT protocols can be very effective.” —Dr. Mohammed Elamir, MD, FACP
A Personal Story of Healing through Aviv Clinics
Using HBOT to address TBIs and concussions has proven to enhance our patients’ vitality, health, and confidence to live their best lives.
Learn about Corey Black’s journey of recovery after sports-related injuries:
Invest in Your Health with the Aviv Medical Program
Good health allows you to focus on the essential areas of your life. The time to invest in your health is now, and the Aviv Medical Program will be with you every step of the way. Contact our team to find out how our treatment plans can benefit you.
Your Health Is Your Wealth: The Importance of Investing in Your Health
The daily choices we make and the activities we engage in impact our quality of life. While health problems and expenses might be an expected norm with age, there are ways you can minimize or even avoid them altogether.
At Aviv Clinics Dubai, we believe making more conscious decisions today will give you the healthspan you deserve. Learn the importance of investing in your health and nine ways to get started.
Note: Speak to your doctor before you pursue any lifestyle changes.
1. Consider the MIND Diet
Eating healthy has been a consistent mantra over the years, and for good reason—there is a connection between diet and disease. A healthy diet is the foundation for feeling good.
While there are numerous diet trends out there, there is one truly worth your time and investment—the MIND diet.
The Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet is a blend of two highly effective diets:
- Mediterranean: Consists of a heart-healthy eating plan
- DASH: Aims to address hypertension or high blood pressure
Studies illustrate the MIND diet is “associated with reduced incidence of Alzheimer’s disease.”
Sticking to this diet that entails a variety of fruits and vegetables provides anti-inflammatory effects on the brain. This impact can strengthen brain cell structure and help regulate anxiety and mood.
2. Engage in Intermittent Fasting
We know—fasting doesn’t sound like the most exciting thing. But consider intermittent fasting. Not only can you achieve a healthy body composition, but you can also improve your brain health—all without strict dietary restrictions.
Intermittent fasting is a dietary lifestyle that comprises alternating periods of eating and fasting and limiting the number of hours you consume calories during the day/week.
This metabolic switching:
- “Promotes neuroplasticity and resistance of the brain to injury and disease”
- May “decrease the progression of Alzheimer’s disease in mice through changes to the gut microbiota”

3. Stay Educated on Fall Prevention Tactics
“Falls in older adults are a reasonably common occurrence.” Conditions that become prevalent as we age (e.g., muscle weakness, osteoporosis, and balance and gait problems) make us more susceptible to falls.
The key ingredient to prevention? Exercise. This entails:
- Strength training
- Cardio training
- Balance training
- Flexibility training
Other fall prevention tactics are just as important.
- Keep your home clear of clutter and trip hazards such as cords, books, shoes, etc.).
- Install grab bars in the bathroom and handrails in the hallways and stairways.
- Avoid wearing clothing that drags on the ground.
- Wear non-slip socks or shoes around the house.
- Take a pause after standing up and before beginning to walk.
4. Find Helpful Ways to Cope with Stress
Stress is inevitable, and the body and mind are biologically equipped to handle it. But sometimes, when the stress gets overwhelming, it can have adverse effects. ”Stress affects not only memory and many other brain functions, like mood and anxiety, but also promotes inflammation.”
Chronic stress can:
- Kill brain cells.
- Cause memory decline.
- Negatively impact mental health.
Whether you are grieving or dealing with a major change in your life, it’s essential to find healthy coping mechanisms for stress:
- Make time for physical activity: At Aviv Clinics, we recommend 30 minutes of exercise three days a week at a minimum. Exercise benefits the brain by releasing endorphins, helping relieve pain, and improving mood. The key is to find an activity you enjoy—this will make exercise fun and feel less like a chore.
- Be conscientious about screen time. Experts say, “The goal isn’t to eliminate screens from your life; it’s to imbue the time you spend on screens with ‘intentionality.’” When used wisely and with purpose, technology offers worthy benefits. But misusing it can cause more harm than good. Thus, stay aware and focus on balancing screen time with other activities.
- Meditate. Not only is meditation a great activity to do instead of “doom scrolling” on your screen, but meditation may promote several benefits such as “reduction of cognitive decline” and “increase in quality of life.”

5. Focus on Body Composition Instead of Weight
A low number on the bathroom scale doesn’t necessarily mean all is well. Indeed, society’s obsession with the scale can lead to problems like declining muscle mass—a condition that will do more harm than good later in life.
So toss that unhealthy relationship with the bathroom scale. Instead, look at your overall body composition.
For example, Aviv Clinics uses the seca scale to get a precise rundown of the meaning behind a person’s weight. This scale helps us develop an accurate and customized treatment plan—losing body fat, gaining muscle, or a combination of both.
Speak to your doctor to gain a comprehensive assessment of your body composition so you can make appropriate, personalized goals.
6. Stick to a Consistent Sleep Schedule
Since the sleep hormone melatonin naturally decreases with age, it’s vital to set up healthy sleeping habits. This entails turning off all electronics an hour before bedtime and getting in bed at the same time each night. Doing so will promote natural circadian rhythms and maintain cognitive health.

7. Engage in Games
Investing in your health doesn’t have to be boring—it can include games!
That’s right, playing brain games is a fun and active way to train your brain. Researchers report “the effectiveness of cognitive intervention in maintaining cognitive health over the long-term.”
The brain functions similarly to muscles building muscle fibers after exercise—it promotes new neurons and neuronal connections after participating in games.
8. Listen to More Music
When was the last time you truly listened to music? What kinds of images and memories did it elicit?
Music offers far more advantages than helping you get through a grueling drive or setting the tone for a party. The best part is these benefits are backed by research.
Studies illustrate music can:
- Improve “cognitive function in people living with dementia, as well as quality of life after the intervention and long-term depression.”
- Reduce “measures of anxiety in a population of residential care patients with dementia.”
- Provide “better sleep quality” for “adults who listened to 45 minutes of music before going to sleep.

9. Find a Research-Backed HBOT Program
Hyperbaric oxygen therapy (HBOT) is a treatment in which the patient breathes 100% pure oxygen in a pressurized chamber. Aviv’s luxury, state-of-the art hyperbaric oxygen therapy suites are the largest and most advance in Dubai and the surrounding region.

Several studies illustrate the potential of HBOT in improving cognitive, physical, and psychological performance when administered in a specific protocol. Aviv Clinic’s HBOT protocol fluctuates oxygen levels during each hyperbaric session. This system increases oxygen levels in the body up to 20 times higher than normal and boosts your brain’s ability to heal.
The unique medical program at Aviv Clinics consists of a treatment program that include this same research-backed HBOT protocol along with cognitive training, dietary coaching, and physical performance training in a physician-designed program tailored to each client’s needs.
This holistic approach gives each patient the personalized care they deserve for their unique health conditions. Our clients have optimized their athletic performance with HBOT and have found relief from debilitating medical conditions such as stroke and traumatic brain injury.
Couple Pursues Healthy Aging & Cognitive Decline Prevention | Bob & Laurie’s Story
Invest in Your Health at DP World’s Aviv Clinics Dubai
The Aviv Medical Program stands by a holistic treatment program that targets all areas discussed above. A series of independent clinical trials illustrate how our program helps treat the symptoms of different health conditions.
6 Future Trends in Healthcare for Patients
As healthcare rapidly evolves, patients must keep abreast of these shifts. Doing so activates your role in driving better health outcomes for yourself and your loved ones.
COVID-19 showed how technology can benefit patients during the pandemic. The medical community in Dubai is leveraging those takeaways to elevate patient care.
Additionally, individuals want to take more ownership of their health through the convenience of personalized, educational, and digital care.
Look out for these six future trends in healthcare throughout 2023 as more healthcare providers take steps to meet patient needs.
1. Remote Patient Monitoring (RPM)
COVID-19 showed how critical technology could benefit patients and elevate care. One way to achieve this has been through remote patient monitoring (RPM).
In 2022, RPM tools (e.g., wearable devices, pulse oximeters, blood glucose meters, and heart monitors) were valued at $53.6 billion. This value is projected to reach “USD 175.2 billion by 2027.”
When “74% of all deaths globally” are attributed to at least one chronic disease, a physician’s ability to remotely manage health conditions is key to preventing hospitalizations—remote patient monitoring (RPM) can reduce “the number of ER visits and hospitalizations.”

2. Health Literacy
With more doctors and patients remotely managing conditions, healthcare organizations are providing digital platforms that offer personalized educational experiences—experiences that address each patient’s health literacy level (in their preferred language and reading level).
As more providers anticipate higher patient volume (from individuals who delayed or avoided medical care during the pandemic and from the return of medical tourism), you’ll see more educational materials at each touchpoint of your care journey.
Don’t hesitate to discuss literacy levels with your doctor to ensure you feel confident and comfortable navigating your health journey.
3. Mindfulness Products
Wellness has taken center stage since 2020, with mindfulness coming to the forefront as an in-demand component:
- McKinsey reports “mindfulness has gained mainstream consumer acceptance relatively recently” among patients. Half of the survey respondents expressed that they wish more mindfulness products and services were available.
- Medical research indicates mindfulnesses exercises such as meditation can reduce “cognitive decline” and “perceived stress.”
Don’t be surprised to see more providers offering holistic care. For example, healthcare organizations may consider partnering with mindfulness apps or providing products that offer mental health benefits.
4. Data Analytics
Objective data is critical to seeing how you’re progressing and what additional steps you and your physician need to take.
More doctors are tracking and sharing with their patients the data that reports:
- Interaction with educational materials
- Treatment and communication gaps that need addressing for better outcomes
- Patient progress along a personalized treatment plan
- Actionable steps a patient takes to manage their health (remotely or in-clinic)
Data transparency helps the provider and the patient understand how a condition is progressing and what can be done to elevate treatment.
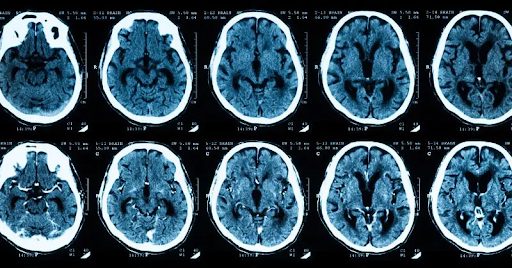
5. Advanced Imaging
The development of new technologies has brought on better ways to treat patients. One prime example is advanced imaging and neuroscience.
Advancements in radiography give medical professionals the tools to perform in-depth assessments of the brain upon a stroke. Advanced imaging may include:
- 3T MRI with DTI (diffusion tensor imaging)
- SPECT scan with new AI analysis methods
These imaging technologies help providers map a personalized recovery plan and track recovery in post-treatment assessments.
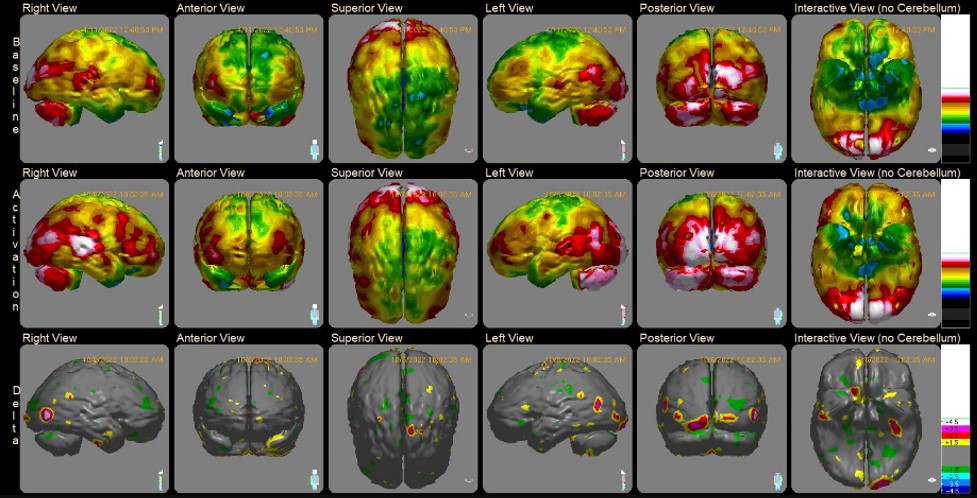
Comprehensive medical programs, such as the one at the Aviv Medical Program, rely on these advanced imaging and neuroscience tools to earn long-term results for stroke patients.
6. Hyperbaric Oxygen Therapy (HBOT)
Oxygen is the lifeblood of our health. As we age, body oxygen levels decrease, leading to infamous age-related decline. While most of these shifts are often thought to be irreversible, research says otherwise.

Studies indicate hyperbaric oxygen therapy (HBOT) can help:
- “Reverse biological aging” by slowing down the growth of cells and protein structures responsible for the aging process.
- “Reverse the main activators of Alzheimer’s disease”
At Aviv Clinics, our unique HBOT program entails fluctuating oxygen levels, which triggers the body’s self-regeneration capabilities.
“By treating vascular dysfunction, we’re mapping out the path toward Alzheimer’s prevention. More research is underway to further demonstrate how HBOT can improve cognitive function and become an influential tool in the imperative fight against the disease.” -Dr. Shai Efrati, Aviv Clinics
Learn More about Hyperbaric Oxygen Therapy
Aviv Clinics Dubai, brought to you by DP World, is here to elevate your healthcare journey, offering the world’s most advanced Hyperbaric Oxygen Program.
Our diverse community of patients has achieved significant health milestones thanks to a multidisciplinary approach that can include:
- In-depth review of health history
- Comprehensive physical exam
- Highly advanced MRI, DTI, and SPECT scans
- Neurological and neurocognitive tests
- Body composition analysis
- Cellular performance analysis
- A detailed report of our assessment findings
- Unique Hyperbaric oxygen therapy (HBOT) protocol
- Cognitive training
- Physical training
- Dietary coaching
- A post-treatment report of your improvements and recommendations for future progress
Our unique medical approach centers on research to provide high-quality care that produces lasting improvements in mental and physical performance. Areas of improvements include:
- Memory
- Concentration
- Information Processing Speed
- Emotional Health
- Stamina
- Energy
- Mobility
- Independence
- Quality of Life
- Sexual Performance (Men)
- Sleep
Benefits of our program also include:
- Stem cells proliferation– the building blocks of tissue rejuvenation – to multiply and migrate
- Lengthen the telomeres – the protective caps at the end of each strand of DNA
- Reduce senescent cells – known to contribute to many age-related diseases
- Increase mitochondrial function – the power plant in each of our cells
If you’ve experienced cognitive or physical decline due to aging or disease, we may be able to help.
To learn more about the Aviv Medical Program, contact the Aviv Clinic.
Treatment for Children and Adolescents with Traumatic Brain Injury (TBI) and PCS
Children and adolescents experiencing the effects of traumatic brain injury (TBI), post-concussion syndrome, and other brain performance problems have the opportunity for a better future with the right approach to treatment. Explore an effective treatment for TBI offered by Aviv Clinics Dubai:
Aviv Clinics Dubai Launches Highly Specialized Youth Medical Program to Assess and Treat TBI and Brain Performance Problems in Children and Adolescents
-
- The program uses Hyperbaric Oxygen Therapy (HBOT) to improve cognitive, emotional, and behavioral symptoms of youth suffering from specific brain-related issues.
-
- The new youth treatment program is backed by a first-of-its-kind study validating the Aviv HBOT protocol as an effective treatment for children suffering from persistent post-concussion syndrome.
-
- The youth program can also help improve the quality of life in children, aged between 8 to 15 years, suffering from cerebral palsy, Traumatic Brain Injury (TBI) and stroke.
- The youth program can also help improve the quality of life in children, aged between 8 to 15 years, suffering from cerebral palsy, Traumatic Brain Injury (TBI) and stroke.


Aviv Clinics Dubai, a wholly-owned subsidiary of DP World, has opened a new wing at its JLT-based specialty brain health and performance center dedicated to a breakthrough Youth Medical Program that uses hyperbaric medicine to treat specific brain injuries in children and youth between the ages of 8 and 15.
The program specializes in the treatment of multiple disorders including cerebral palsy (a childhood motor disorder in childhood caused by brain injury due to lack of oxygen or blood supply), Traumatic Brain Injury (sudden damage to the brain caused by a blow or jolt to the head), and strokes (when the blood supply to part of the brain is cut off, because of a blockage or a blood vessel rupture).
The Aviv Youth Medical Program is the focus of a new study, published in Nature Scientific Reports, which shows the effectiveness of Hyperbaric treatment in healing damaged brain tissue and alleviating symptoms in children experiencing persistent post-concussion syndrome (PPCS), where concussion symptoms continue beyond the expected recovery period.
The study, conducted at the Sagol Center for Hyperbaric Medicine and Research at Shamir Medical Center, suggests that HBOT improves cognitive and behavioral function, as well as quality of life in pediatric patients suffering from PPCS, even years after receiving their traumatic injury.
The Aviv Youth Medical Program treatment starts with a comprehensive three-day medical, physiological, and mental assessment carried out by Aviv-certified medical staff including pediatricians, pediatric neuropsychologists, physical therapists, speech therapists, occupational therapists, and nurses. This includes the most advanced brain imaging tests suited to the child’s needs, such as perfusion MRI, and SPECT.
After analyzing the results of the in-depth assessment, children undergo HBOT sessions five days a week for 12 weeks – 60 consecutive one-hour sessions in total. Alongside the HBOT sessions, the patient will receive personalized cognitive and physical training designed to maximize the effects of the rehabilitation. At the end of the treatment, tests are repeated and compared with the results of the initial assessment.
“The diagnosis and treatment of post-concussion syndrome in children is a critical issue that physicians and researchers have struggled with, to the detriment of the children,” said Dr. Shai Efrati, Medical Director of the Sagol Center for Hyperbaric Medicine and Research and Shamir Medical Center, and Chair of Aviv Scientific’s Medical Advisory Board.
“For the first time, we have demonstrated an effective treatment for pediatric PPCS, whether the injury occurred six months or 10 years ago. This discovery and the launch of our new Youth Medical Program offers hope to thousands of families watching their children suffer from unrelenting symptoms.”

Upon completion of the study, researchers found that children treated with HBOT experienced a significant improvement in cognitive function, including the general cognitive score, memory, and executive function (ability to plan, prioritize tasks, and complete complex goal-directed behaviors), compared to the untreated children.
Other PPCS symptoms that improved include behavioral symptoms such as hyperactivity, and, perhaps most strikingly, the study revealed parallel structural brain changes, as seen on MRI, in the areas of the brain known to be affected by TBI leading to cognitive dysfunction and other symptoms of PPCS.
“Working in collaboration with DP World, we are able to bring to Dubai and the UAE medical community this highly specialized brain performance program grounded in more than 15 years of research and powered by truly state-of-the-art technology. As this study shows, we have the potential to give new hope to our young people and their families through the ability to diagnose and treat what can be debilitating symptoms of TBI, as well as other common brain disorders such as Cerebral Palsy and strokes. At the same time, we are able to contribute to advancing both Dubai’s and the UAE’s positions as global innovators and hubs for med tech and medical tourism,” said Mike Frayne, CEO of Aviv Clinics Dubai.
The same treatment protocol conducted during this study will be adopted in the youth wing at Aviv Clinics in Dubai. It will be administered under the same strict protocols, with additional comprehensive cognitive and physical training support for the various conditions and symptoms addressed by Aviv including concussion and TBI, and more. Aviv Clinic’s new Youth Medical Program is located in a dedicated wing of the 7,000-square-meter, state-of-the-art brain health and performance clinic in Dubai’s JLT.
If your child needs treatment for TBI symptoms or other brain conditions, we encourage you to learn more about the Youth Medical Program at Aviv Clinics Dubai by DP World.
The Key to Healthy Aging: Hyperbaric Oxygen Therapy vs Stem Cell Therapy
The transitional time we all experience after retirement age can feel tough, scary, depressing, and isolating. We begin to miss the “good old days” when performing at our peak was easy and rewarding. But please know that there is hope.
Science has advanced so much over the past decade and has delivered some promising therapies. Two of them have been gaining notable attention: stem cell therapy and hyperbaric oxygen therapy (HBOT). You may not be very familiar with either one, but they have enhanced human biology over the years.
Stem cells are one of the most important and impressive parts of the body. Every organ requires them to maintain optimal function and performance. To keep your body functioning, stem cells self-replicate, having “the remarkable potential to renew themselves” although they do so at a much higher rate when you’re young. As you age, stem cells have “restricted self-renewal potential” and gradually lose their self-renewal capabilities.
However, there’s a way to organically increase the number of stem cells in your body for the purpose of healing and healthy aging.
We’re not talking about a beauty regime that involves injecting stem cells into body parts for a more youthful appearance. We are talking about something far more effective at reverse aging—using a scientifically-backed hyperbaric oxygen therapy protocol to nurture your body’s own stem cell reproduction in your brain.
There’s no question — everyone can benefit from having their brain grow more stem cells. This guide lays out all the key facts on how to trigger your body to reproduce its own stem cells in Dubai. Aviv Clinics brought to you by DP World, walks you through the key details.
What Are Stem Cells?
Stem cells are the body’s internal repair system. When our cells go through normal wear and tear, injuries, or diseases, stem cells develop replacements for lost or damaged cells.
The incredible thing is that stem cells are like 3D printers of the body—they can develop into almost any type of cell in the body, from muscle to brain, and can repair and “recreate functional tissues.”
Our body is like a machine. In the beginning, when we are young, our machine works well—we have numerous stem cells. But as we age, the ability to do this starts to decline: Stem cells’ “renewal ability deteriorates and their ability to differentiate into the various cell types is altered.”
“As the amount and potency of stem cells start to decline…we start to lose tissue. This is what we call aging.” – Dr. Shai Efrati, MD, Director of Sagol Center for Hyperbaric Medicine and Research.
Given the powerful abilities of stem cells, researchers have studied them for decades to discover therapies for aging-associated disorders.
How Does Stem Cell Therapy Work?
Stem cell therapy renews damaged organs, tissues, or bodily functions. It’s an invasive therapy that physicians administer through:
- Injecting stem cells into the bloodstream
- Directly injecting healthy stem cells into a specific area of the body (e.g., the knee)
- Engraftment—when transplanted stem cells grow in the body and reproduce healthy blood cells
Uses of Stem Cell Therapy
Stem cell infusions and transplants are used for repairing cells damaged by chemotherapy or certain types of disease. Examples of these conditions include Leukemia and radiation injury.
Because of the“plasticity [and] self-renewal” abilities in stem cells, researchers note stem cell therapy “could delay or even reverse aging.” However, more studies need to be done to discover a specific stem cell treatment for reverse aging.
Limitations and Dangers of Stem Cell Therapy
Though stem cell therapy has made a lot of progress in health and wellness, there are limitations and potential risks to keep in mind:
- First and foremost, quality evidence is limited for the clinical improvements of stem cells therapy for most possible applications on humans.
- Currently, it is not possible to generate stem cells in large quantities. There isn’t a solution available to “generate large quantities of stem cells” in a laboratory. This makes stem cells difficult to obtain and purify.
- Stem cell therapy is limited to certain conditions.
- Stem cells therapy is an invasive procedure and therefore harbors the hazards of any invasive therapy, such as infections and the risk of significant local and system reactions, which could pose a significant health risk to the recipient.
While stem cell therapy has made its presence in Dubai, it is still very much in the research phase, which does limit its use as an effective therapy for age reversal.
Is HBOT Stem Cell Therapy?

Many people ask this question, but no. Hyperbaric oxygen therapy (HBOT) is not stem cell therapy. Rather, HBOT is a method that triggers your body to multiply its own stem cells organically.
Here’s how that works:
- Oxygen is your brain’s superpower. Every bodily function depends on it, including the reproduction of stem cells.
- As we age, our bodies are less efficient at channeling oxygen to the areas we need it most (e.g., brain tissue). This is why we “slow down” over time, both mentally and physically. We’ve come to accept this as the norm and assume there’s nothing to be done about it.
Luckily, science says otherwise.
Nobel Prize-winning research reports that hypoxia is a strong stimulator for triggering stem cell proliferation and regeneration processes. These stem cells can enable our brains and bodies to regain their peak performance levels.
The Aviv Clinics treatment protocol utilizes the hyperoxic-hypoxic paradox in order to gain the benefits of hypoxia without having to expose patients to a true lack of oxygen and the risks involved.
Uses of Hyperbaric Oxygen Therapy
People have historically used hyperbaric oxygen therapy to treat a variety of conditions that involve oxygen-starved tissue. These include:
- Wound healing
- Delayed radiation injuries
- Carbon monoxide poisoning
The promising results of HBOT have prompted many physicians and scientists to dive further into research to identify possible impacts the therapy has on reverse aging and other health areas.
Landmark Research on a Hyperbaric Oxygen Unique Protocol
Founded on decades of research, it’s proven that unique hyperbaric oxygen fluctuations encourage the body to multiply its own stem cells. This specific protocol targets various health and wellness areas, such as:
- Reverse aging: Landmark research shows success using HBOT for reverse aging. Now, many doctors refer to HBOT as the scientific “Holy Grail.” The therapy has helped many individuals improve their cognitive and physical performance.
- Post-stroke rehabilitation: HBOT helps restore function of injured brain tissue in survivors.
- Traumatic brain injuries (TBIs): Studies illustrate HBOT can “induce neuroplasticity”—the brain’s ability to change and adapt. This potential can help repair damaged brain functions for those suffering from challenges after traumatic brain injuries (TBIs).
Limitations and Dangers of HBOT
- Not all HBOT administration is the same across clinics. Some use monoplace oxygen chambers, while others use multiplace chambers. Also, the way oxygen is administered is different across clinics as well. For example, most clinics administer oxygen at a steady level rather than use the oxygen fluctuations required to gain the benefits (based on Nobel-prize winning research).
- HBOT is an elective treatment. HBOT in the context of Healthy Aging is not covered by insurance.
- Potential side effects due to pressure changes may include ear and sinus discomfort. For some chronic conditions, special considerations may be needed.
The Aviv Medical Program’s Role in Stem Cell Proliferation

The Aviv Medical Program in Dubai prescribes HBOT to activate the body’s regeneration mechanisms — this helps regenerate more stem cells.
Stem cell growth in your brain helps:
- Grow new brain matter, increasing both the quantity and quality of healthy cells.
- Produce neuroplasticity, improving the quality of nerve fibers in the brain and other organs in the body.
- Boost your body’s own ability to heal wounds, including injured tissues resulting from a stroke or traumatic brain event.
These three developments ultimately drive new blood vessels to form, help restore injured tissues, and improve wound healing throughout the body.
Imagine your aging body feeling far better than it did years ago. Achieving higher cognition levels, improving athletic performance, and finally finding relief from conditions such as traumatic brain injuries, post-concussion syndrome, fibromyalgia and stroke is part of the program.

How Does it Work?
- You enter a technically-advanced room known as an Hyperbaric Oxygen (HBOT) suite and put on a mask to breathe 100% pure oxygen that is pressurized to above atmospheric levels. This increases oxygen levels in the body up to 20 times higher than normal, sending the boosted oxygen to deprived tissues in the brain and throughout the body.
- Aviv Clinics health professionals fluctuate the oxygen levels. These fluctuations trigger stem cells to multiply and new blood vessels to develop. While other clinics typically focus on injecting the body with types of stem cells, Aviv Clinics’s unique protocol fuels the body to reproduce stem cells organically.
- Alongside other cognitive, physical, and nutritional training you undergo as an Aviv Clinics client, you’ll see significant improvements in your mental and physical performance. Your body’s natural healing and regeneration process will be turbocharged.
You’ll walk into the Aviv Clinic curious and perhaps a little apprehensive. You’ll leave confident and ready to live life to the fullest — no matter your age. Your work, physical activity, and emotional connection with those you love will come easier than it has in years.
Why Hyperbaric Oxygen Therapy at Aviv Clinics Dubai May Be a Better Alternative to Stem Cell Therapy
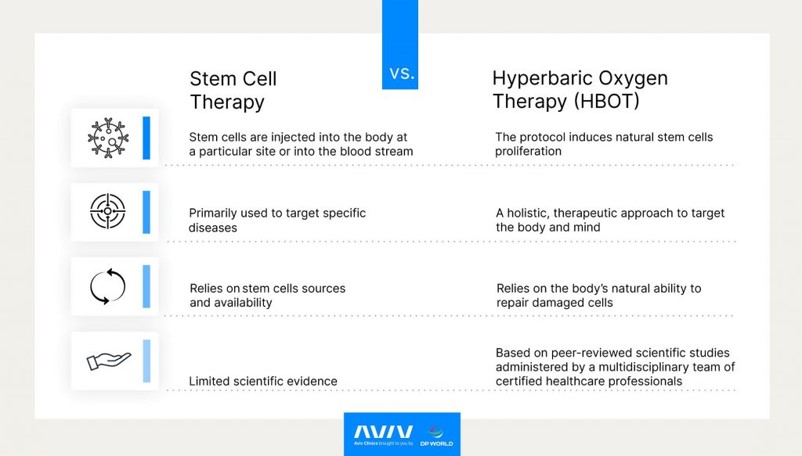
HBOT offers a safer, scientifically backed and a much more reliable approach to improving cognitive and physical performance (reverse aging), post-stroke rehabilitation, and traumatic brain injury.
Again, stem cell therapy currently does not have enough high quality data to know if it is an effective reverse aging treatment.
While stem cell therapy is invasive, HBOT is non-invasive, which means that there is no risk of acquiring infections or other side effects associated with invasive procedures. Individuals breathe in 100% oxygen, usually through a mask, and HBOT triggers the proliferation of your own stem cells.
The natural approach HBOT takes is why so many people have been able to experience long-term, systemic improvements throughout the entire human body. HBOT targets both the brain and body to improve the aging process and quality of life.
To explain further:
- Stem cell therapy is an invasive therapy (stem cells are injected into the body). HBOT is non-invasive. Aviv Clinics’ HBOT process is administered via an oxygen mask in a first class multi-person suite, and the oxygen fluctuations trigger the body’s ability to naturally proliferate its own stem cells.
- Aviv Clinics’ HBOT protocol is founded on decades of research and offers a holistic therapeutic approach to target the brain and body, enhancing overall human performance and aging. As far as stem cell therapy is concerned, high quality data is still not sufficient to fully understand the relevance of this treatment.
- While the success of stem cell therapy relies on stem cell sources and availability, HBOT at Aviv relies on the body’s natural ability to repair damaged cells. This offers a safer and more reliable option to boost performance and limit aging in the long run.
- HBOT at Aviv is based on peer-reviewed scientific studies.
Learn more about the science of hyperbaric oxygen therapy
3 Conditions Aviv Clinics Can Help Treat with Natural Stem Cell Proliferation
Many systems and functions in the brain and body can be improved when HBOT fluctuations trigger the body’s own ability to proliferate stem cells organically in the brain and other organs. Now we’ll touch on some of the conditions we help treat here in Dubai.
1. Anti-Aging
Landmark research shows it’s possible to use HBOT for reverse aging at the basic cellular-biological level. Now doctors use HBOT as the scientific “Holy Grail.”
Watch how Dr. Joe Maroon, Vice Chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center, saw significant results in his physical and cognitive performance after HBOT.
2. Stroke
When a stroke occurs, part of the brain is cut off from its blood supply and oxygen. That’s when cells begin to die.
Up to 50% of post-stroke survivors suffer from motor dysfunction (balance, hand control, etc.) and/or brain impairment (memory loss, inability to focus or reason, etc.).
Fortunately, there is hope for stroke recovery with stem cell production using HBOT and other cognitive and physical therapies. This holistic treatment plan rejuvenates injured brain tissue and helps to restore function.
Watch the story of Keren Trabelsi (mother and business owner) on how getting treated at Aviv Clinics after suffering a stroke accelerated the recovery of her physical and cognitive abilities.
3. Brain Injury
Whether you’ve suffered from a traumatic brain injury (TBI) or know a loved one who has, you know how devastating the effects can be. The damage TBI can cause includes restricted blood flow to brain regions and impaired brain tissueA.
Studies illustrate HBOT can induce neuroplasticity in the brain and repair damaged brain functions, ultimately “improving brain function and quality of life.”
Watch Linden Perry’s story about using HBOT stem cell production for a brain injury to heal her lingering health conditions after sustaining a concussion as a goalkeeper on her soccer team.
Enhance Your Quality of Life with DP World’s Aviv Clinics Dubai

The Aviv Clinics brought to you by DP World in Dubai is a leader in enhancing physical and cognitive performance for the long term. We utilize highly-advanced HBOT protocols to help your body organically reproduce its own stem cells.
Whether you want to climb a mountain or simply get on the floor to play with your grandchildren, maintain the ability to perform complex work or have more connecting conversations with your loved ones, there’s help for you here. Be a part of this advanced scientific breakthrough for healing the mind and body from aging, stroke, and brain injury.
For a complete assessment to see if you are qualified for our treatment program of proliferating stem cells in Dubai, contact us today.
Schedule a Consultation to Learn More About Aviv Clinics
The unique HBOT protocol at Aviv Clinics is founded on decades of research. If you’re looking to reverse your biological age and naturally proliferate your body’s stem cells, the Dubai team is on your side. Schedule a free consultation with Aviv Clinic in Dubai to satisfy your curiosity about how hyperbaric oxygen therapy can benefit you!
How to Help a Stroke Victim Recover: 5 Actionable Steps to Take
There is no other way to put it—seeing your loved one lose their independence after a stroke is difficult. Though you may not be able to control the situation, what you can control is the support you offer. This is where we come in.
The Aviv Medical Program offers five actionable ways to help your stroke victim recover. The goal is to equip you with practical tips and effective support to help you feel more confident as a caregiver, allowing you to guide your loved one through a smooth post-stroke recovery journey.
The Possible After-Effects of a Stroke
Some common post-stroke effects you may witness include physical, cognitive, and emotional symptoms.
Physical Effects
- Lack of ability to feel objects (e.g., holding an object is difficult)
- Pain, numbness, tingling/prickling, or heaviness of limb
- Loss of bladder and bowel control
Cognitive Effects
- Aphasia (loss of ability to speak, write, and understand spoken/written language)
- Decline in memory, learning, and awareness
Emotional Effects
- Sense of fear, anxiety, frustration, or depression due to loss of physical and cognitive ability or brain damage
5 Things You Can Do to Help a Stroke Victim Recover
When day-to-day capabilities are suddenly taken away, it’s challenging for your loved one to find the will and a path forward to a better life. We encourage you to be patient with each step — every person is different. Thus, there is no solid timeframe for when you’ll see improvement.
Here are five actionable things you can do to help.
1. Learn About Their Stroke, Symptoms, and Treatment Plan
Stroke incidents impact individuals in different ways. Before crafting a support plan, take time to understand their stroke, symptoms, and therapy program(s). This is pivotal to providing the right kind of support.
Learning about your loved one’s condition may involve:
- Sitting with them during doctor and therapy appointments
- Learning the physical impacts that have occurred (e.g., what areas of the brain are affected and how much of the brain has been impacted by the stroke)
- Understanding the type of therapy they need and why
2. Maintain a Safe and Accommodating Environment
Once you’ve acquired a good understanding of your loved one’s stroke, symptoms, and treatment plan, ensure their home environment aligns with their health conditions.
For example:
- If your stroke survivor experiences visual and sensory difficulties, you may need to move objects around their room accordingly. For instance, having trouble seeing or feeling things on their left side may merit moving all of their items to their right side.
- Ensure pointed edges on furniture and doorways are protected. This should especially be the case if your loved one is having difficulty moving around on their own or is experiencing physical ailments.
3. Respect Their Needs, But Don’t Do Everything
Help your friend or family member when they ask for help. Do not step in and do tasks for them. Some stroke patients are trying to regain their independence, so it helps to give them the space to do things on their own if they prefer.
Speak with an occupational or physical therapist or speech-language pathologist to ensure the ways you are helping your loved one are safe and abiding by the recovery plan.
4. Offer Emotional Support
Many people primarily think about the physical and cognitive repercussions that can come with a stroke, but several “invisible” or emotional factors lie beneath the surface.
Anxiety and depression are common in stroke survivors – about one in three stroke patients experience them during the first year after a stroke. The loss of freedom from a stroke is a significant change, and your loved one may express their grief and emotions in various ways (e.g., withdrawing from others, expressing anger, etc.).
Understand that these emotions are a normal part of the recovery journey. Don’t tell someone how to feel or what to do; offer a listening ear and help them however they need it.
5. Stay Centered on a Holistic Approach
A holistic treatment plan is key to helping your loved one recover.
For example, the Aviv Medical Program offers post-stroke recovery treatment that can entail a customized combination of the following:
- Hyperbaric oxygen therapy (HBOT)
- Physical training
- Cognitive training
- Nutritional coaching
Take former stroke patient Cindy for example. After undergoing a personalized hyperbaric oxygen therapy program, she can again walk comfortably, feel sensation in her left hand, engage in cognitive activities. Cindy regained her independence and many physical and cognitive functions she’d been lacking for years after her stroke.
Discover Cindy’s post-stroke recovery story. For her, this new stroke treatment worked a miracle.
“It didn’t take long at Aviv before I was able to get the courage to try things. And now, that fear is almost, I’d say 95% gone. I wanted to be able to comb my hair. I wanted to drive. And yes, because of Aviv, I am able to do those things — and it has changed my life.”
3 Things to Watch Out For During Recovery from a Stroke
There are a few things to keep in mind to ensure the most successful post-stroke recovery journey.
1. The Likelihood of Having Another Stroke
Research indicates stroke recurrence is the highest within the year after the initial stroke. Efforts at prevention should be initiated as quickly as possible.
If your loved one has any of the following conditions, they are at an even higher risk of having another stroke. Be sure these conditions are managed by a doctor.
- High blood pressure
- High cholesterol levels
- Heart disease
- Diabetes
2. Falls—Don’t Ignore Them
Falls are common after a stroke. As falls can cause further damage and prolong recovery, it’s essential to take your loved one to the hospital after a fall incident.
Some critical signs to look out for include:
- Pain, bruising, or bleeding after a fall
- Two or more minor falls within six months
A physician or physical therapist can assess your friend or family member and make any needed adjustments to the treatment process.
3. Self-Care
Taking care of someone involves a lot of patience, effort, and time. Thus, periodically check in with yourself.
How are you feeling? Do you have the right self-care resources to nurture your mind and body and continue caring for your loved one?
Caring for someone begins with you, so don’t forget to look after yourself.
Where to Get Support When Helping a Stroke Victim Recover
If your loved one needs extra support, find the best stroke rehabilitation center near you to provide unique, research-backed protocols—plans tailored to fit the needs of the individual.
Aviv Clinics Dubai offers the latest advances in examining and improving cognitive and physical performance. This includes HBOT. Our state-of-the-art HBOT treatment suites provide intermittent oxygen levels that help the body heal even years after a stroke incident.
Focused, repetitive practice is key to successful recovery, which is exactly what we offer each patient.
New Stroke Treatments Work Miracles at Aviv
Aviv Clinics brought to you by DP World knows how to help a stroke victim recover. We don’t simply provide a unique medical protocol backed by decades of research—we offer a supportive group of professionals who will be with you at every step as you help your loved one find relief.
Contact us to get in touch with a personalized team of medical staff at the best stroke rehabilitation center in UAE.
The 5 Support Stages of Brain Recovery After a Stroke
The brain is a powerful yet delicate organ that carries out numerous functions—functions we often take for granted.
Having a stroke can cause debilitating injuries to the brain, yet the aftermath can be even more challenging to your health and lifestyle. Up to 50% of stroke survivors suffer some form of motor dysfunction or brain impairment—including memory loss, difficulty focusing and processing information, and an inability to reason.
No one wants to have their most significant capabilities suddenly stripped away. That’s why we’re here.
If you do not feel the same as you did before your stroke, the Aviv team has answers. The time to commit to your health is now. Learn the five stages of brain recovery after a stroke and the treatment options available to you.
What Happens to the Brain During a Stroke?
Blood carries oxygen and essential nutrients that nourish brain cells. But during a stroke, blood cannot reach crucial parts of the brain. The main types of strokes:
- Ischemic stroke: Blood clots, fatty deposits (plaque), or other particles block the blood vessels to part of the brain.
- Hemorrhagic stroke: Weakened artery in the brain leaks blood or ruptures, putting too much pressure on brain cells and damaging them.
- Transient ischemic attack (TIA): Not a true stroke (often called a mini stroke, silent stroke, or warning stroke).
Ischemic strokes make up 87% of all strokes (including TIAs), with hemorrhagic comprising the other 13%.
In either case, sections of the brain become damaged, which can manifest cognitive, physical, and even emotional symptoms.
How the Brain Recovers from a Stroke: The 5 Stages of Support
Research illustrates the brain can reorganize and adapt in response to injury. That means there’s hope for stroke survivors because the brain can be retrained.
Now, post-stroke recovery is not as cut and dry as one would hope. Because every person has different stroke symptoms, lifestyles, and health backgrounds, it’s important to find a post-stroke recovery plan created solely for you.
Here are the five stages of post-stroke recovery. Each stage represents a milestone that gets you closer to living a better, more fulfilling life. The right treatment plan will include one or a combination of these post-stroke rehab therapies.
1. Thinking, Memory, and Perception
Neuropsychologists look at the link between someone’s brain and their potential to participate in daily activities. Neuropsychologists typically conduct an assessment to measure areas such as memory, learning, and processing speed.
The doctors can identify which areas of the brain have been most affected and will provide a rehabilitation plan based on the data.
2. Communication and Language
Social interactions lie at the core of human life. So when this is taken away through aphasia (a disorder that impacts a person’s ability to understand or express speech), communicating with friends and family becomes extremely difficult and frustrating.
Stroke patients with aphasia are often referred to speech-language pathologists (SLPs). SLPs help individuals relearn speech and communication techniques, such as controlling mouth and throat muscles and engaging in cognitive language exercises.
Early speech intervention often leads to improved communication skills at the 12- and 26-week marks.
3. Exercise and Mobility
Exercise and mobility may entail working with a physical therapist—someone who helps you move more easily and ease some of the pain. This recovery program includes movement exercises along with balance and breathing techniques. All of this helps patients reacquire motor skills and get back to their normal routines.
Studies show consistent physical therapy decreases the risk of hospital readmission in post-stroke patients.
4. Healthy Diet
Diet plays a vital role in how we think, feel, and move. Dietitians can be beneficial to post-stroke patients. Here’s why:
- Upon a stroke, some stroke patients experience feeding and swallowing problems. They may also experience loss of appetite. These conditions can impact patients’ weight and nutritional intake.
- Dieticians can make specific recommendations based on your needs to improve your health and minimize the risk of having another stroke.
5. Hyperbaric Oxygen Therapy (HBOT)
Several studies have clearly shown the benefits of using oxygen fluctuations in post-stroke recovery. Aviv’s HBOT therapy process has patients sit in a pressurized environment, breathing in 100% oxygen. Our experts adjust oxygen fluctuations that trigger the self-regenerative mechanism of the body for impressive results.
Not only does HBOT elevate oxygen in the body, but our program promotes neuronal brain cell rehabilitation that can result in:
- Regained speech
- Recovered ability to read and/or write
- Restored motor function
- Return to independence in performing daily activities
Case Study: Keren Trabelsi
The key to successful stroke recovery is through a holistic treatment plan that nourishes your mind and body along an effective and long-lasting recovery roadmap.
The good news? You can find this at the Aviv Medical Program. Our post-stroke recovery treatment program can combine cognitive, physical, dietary, and HBOT training.
Former patient Keren Trabelsi suffered an ischemic stroke, which caused paralysis on the left side of her body. Furthermore, lingering cognitive issues made daily tasks difficult and crushed her well-being.
Luckily, Keren found the Aviv Medical Program and underwent a comprehensive treatment plan. Thirteen months later, she can walk comfortably, feel sensation in her left hand, and engage in cognitive activities (i.e. crossword puzzles, Sudoku, etc.).
“[The Aviv Medical Program is] like driving a Ferrari on the road to recovery versus driving like an old beaten-up car…”
Learn more about her post-stroke recovery below.
What You Need to Know About Post-Stroke Recovery
There are a few things to keep in mind to ensure the most successful post-stroke recovery journey:
- Several factors influence recovery. These are different for everyone and include:
- Where in the brain the stroke occurred
- How much of the brain was impacted
- The survivor’s will and motivation to improve
- Level of caregiver support
- The quality of a rehabilitation program
- “Carefully directed, well-focused, repetitive practice” retrains the brain and is essential to any neurorehabilitation program. It’s the same concept as if you were to learn a new skill like playing a musical instrument.
- Patients and healthcare professionals should be especially vigilant in preventing another stroke from occurring. This requires beginning treatment right away. It also entails monitoring the following conditions as they can put you at higher risk for another stroke:
- High blood pressure
- Heart disease
- High cholesterol
- Diabetes
- Measuring progress matters. Working with a medical staff that captures and tracks data is critical to your success. This allows doctors to adjust treatment as necessary to get the best results possible.
For example, the Aviv Medical Program leverages analytics to produce a report of your health and progress. This may include brain stroke images and MRIs. The data gathered from these analytical tools enable our team to make the right adjustments and give you precisely what you need to elevate your quality of life.
2 Main Signs of Post-Stroke Recovery
Listed below are two signs of post-stroke recovery. If you find that your journey is a little different, don’t stress about it. Everyone’s circumstances are different; thus, timelines and progress will vary.
- There is progress within three months and beyond. Though everyone recovers from a stroke at a different pace, the first three months are generally when patients see and feel the most improvement.
- Independence is improving. After a stroke, you may become more dependent on others to fulfill daily-living tasks such as getting dressed, bathing, or eating. With the right post-stroke recovery plan, you’ll begin to rely less on others and start performing those tasks independently again.
New Stroke Treatment Works Miracles at the Aviv Clinic
It’s time to return to optimal health. If you or your loved one has undergone a stroke (either recently or years ago) and is looking for scientifically advanced stroke recovery therapy, contact Aviv Clinics. We’ll put you in touch with our medical team who provides comprehensive assessments of every stroke patient.
Our team takes pride in helping a diverse array of patients. Rest assured, we will work with you one-on-one to craft an individualized plan. Learn more about our Aviv Clinics brought to you by DP World.
10 Signs and Symptoms of a Mild Stroke: Are You Suffering Without Realizing It?
You’re probably familiar with common stroke symptoms — difficulty speaking, seeing, walking, and numbness on one side of the body. These are all obvious signs, enabling you to quickly get the help you need.
However, it’s possible to have a stroke and not even know it or remember it happening. Silent cerebral infarction (SCI) and Transient ischemic attack (TIA) is a “mild stroke” that causes brain damage and can to a more severe stroke down the road, possibly within the next year.
Mild strokes (also called “silent strokes” or “mini strokes”) are much more common than other recognizable types of strokes. The Rotterdam Scan Study found that 25% of brain scans done on 1,077 elderly patients had signs of a stroke, with 80% of those patients not knowing they had suffered one.
In population-based studies, silent stroke symptoms (silent brain infarcts) on MRIs have shown the following prevalence:
- 8% to 31% for white, Black, and Japanese populations
- 10.7% to 84% for those aged 53–71 years
- An increased risk for men and younger Black populations
Canadian researchers have discovered that mild strokes are “common in seniors after they have elective, non-cardiac surgery” which leads to a doubled “risk of cognitive decline one year later.”
How a Mild Stroke Differs
Just as with other types of strokes, a mild stroke occurs when the blood supply is cut off to part of your brain. The difference is that the part of your brain affected by a mild stroke is too small to hamper the control of your vital brain functions, so symptoms may go unnoticed or be blamed on other health or mental conditions.
Most people won’t positively know that they’ve had a mild stroke without an MRI or CT scan picking up on affected small blood vessels, changes in white matter, or lesions.
Still, the signs and symptoms of a mild stroke shouldn’t be ignored.
A mild stroke does kill brain cells and tissue and should be caught in order to treat symptoms and prevent another stroke from taking place. It’s not uncommon to suffer several mild strokes before noticing a cumulative neurological effect, even vascular (post-stroke) dementia. In fact, up to one-third of those who suffer from a stroke develop dementia within six months.
The Cleveland Clinic Abu Dhabi urges residents to look for mini stroke warning signals.
Why? Because “while the global average age of a stroke victim is over 65, the average age in the UAE is younger due to the high prevalence of risk factors such as obesity, high blood pressure and diabetes. Half of all stroke patients in the country are under the age of 45.”
So, what are the signs and symptoms of a mild stroke? Here’s what might tip you off to the root cause of your symptoms.
The Most Common Signs and Symptoms of a Mild Stroke
Up to 50% of stroke survivors suffer from motor dysfunction or brain impairment. Here are 10 signs of a mini stroke you or a loved one may experience suddenly but mildly, and which may last a couple of hours, a few days, or long-term:
- A lapse in or loss of short-term memory: Do you have to ask someone to repeat instructions they just told you but still remember details from a conversation you had last month? Is there a day or activity you had recently that you simply don’t remember, even with prompts?
- A decreased ability to think or reason: Have you given up on a game you used to love playing, like Sudoku or crossword puzzles? Do you find yourself frustrated or arguing more because you don’t understand someone else’s reasons for wanting you to do something?
- Mood changes: Are you suddenly irritable, anxious, apathetic, or depressed? Have you found yourself crying or laughing for no obvious reason or at inappropriate times?
- Psychiatric disorders: Do you have hallucinations or delusions? Have you found yourself engaging in inappropriate motor behavior, like nibbling food at the dinner table or repeatedly banging your head?
- Trouble with balance: Are you experiencing dizziness or feeling like your head is spinning? Is it difficult to make quick adjustments to maintain balance? Do you find yourself stumbling or bumping into things? Does it feel like you’re standing upright when in fact, you’re leaning to one side?
- Movement or walking impairment: Are your toes now catching on the ground when you take steps? Do you tire easily just from walking to your neighbor’s house? Is walking and talking at the same time difficult for you?
- Limb clumsiness: Does it take concentration to control your hand motions? Is it tricky to type even though you’re normally very proficient? Do you have a shaky leg? Are you noticing a decrease in hand-eye coordination?
- Incontinence: Do you feel the urge to urinate more often than usual? Are you consciously or unconsciously leaking urine or stool during the day or while asleep at night? Is it difficult to empty your bladder completely?
- Headaches or migraines: Are you having more headaches or migraines than usual? Or are you getting long-term, persistent headaches? Have your headaches become severe enough to disrupt your daily activities?
- Vision issues: Does seeing things clearly take concentration? Are you less aware of your surroundings? Are you having double vision? Has your field of vision reduced?
It’s important to note that these symptoms of mild stroke may also be signs of other medical conditions, so it’s important to speak with your doctor about your concerns and treatment options.
Stop Suffering in Silence: Schedule a Consultation
The truth is, there is no such thing as a mild stroke, as their symptoms are real and can have long-lasting, significant effects on your body and life.
Don’t suffer in silence. If you or a family member are showing signs of a mild stroke, there is hope. A customized post-stroke recovery medical program utilizing advanced HBOT techniques helps heal the brain and body, leading to a remarkable recovery and lowered risk of suffering a serious stroke in the future.
Schedule a complimentary consultation with a doctor at Aviv Clinics brought to you by DP World or take a tour of our specialty clinic and get your advanced brain imaging scans to check for symptoms of a silent stroke.
5 Ways to Maintain Healthy Cognitive Ability as You Age
You want to stay sharp as you get older, we get it. Everyone hopes to age gracefully and enjoy their golden years full of new experiences and good memories. But as you know, this doesn’t always happen. Some people, as they grow in years, lose mental clarity and ability. Often this happens so gradually that it’s like watching hair grow—a loss of cognitive ability isn’t even noticed until it’s too late to do much about it.
But don’t worry, there is plenty of good news.
There are scientific, practical ways to help you maintain optimal brain health as you get older. As a health and industry leader in cognitive and physical performance, Aviv Clinics provides valuable, research-backed information to help you control your cognitive ability long into your twilight years.
5 Categories of Cognitive Skills You Want to Maintain
When we talk about cognitive ability, what we’re referring to is a set of seven skills that work together to help you in your daily life:
- Short-term memory
- Long-term memory
- Attention—sustained, selective, and divided
- Processing speed, including visual and auditory
- Logic and reasoning
Our brains can do brilliant and beautiful things! We simply need to nurture their natural abilities, so we can slow (or prevent) mental decline.
How to Improve Cognition – Follow Your Doctor’s Orders
Knowing how to improve cognitive skills is the first step toward achieving your goal of staying sharp and full of life for many years to come.
First, are you at risk of cognitive decline as you age?
- Do you have depression?
- Are you lacking sufficient mental activity?
- Are you avoiding physical exercise?
- Would your doctor consider you obese?
- Do you have high blood pressure?
- Have you been diagnosed with Type 2 diabetes?
- Are you a smoker?
To significantly lower your risk of cognitive decline, follow your doctor’s orders and incorporate these five must-have lifestyle adjustments to enhance your cognitive ability.
1. Sink Your Teeth into a Delicious Mediterranean Diet
Good nutrition goes a long way in maintaining a healthy brain and body. Studies show an association between high adherence to a Mediterranean diet and reduced risk of Alzheimer’s disease.
A Mediterranean diet entails:
Eating plenty of:
- Fruits and vegetables
- Fish and seafood
- Nuts and legumes
- Whole grains
- Unsaturated oils (extra-virgin olive oil and avocado oil)
Eating in moderation:
- Poultry
- Eggs
- Cheese
- Yogurt
Eating rarely:
- Red meat
- Refined grains
- Added sugar
- Highly processed foods
Read MIND Your Diet for Better Brain Health for some very interesting and informative guidance from an AVIV dietician, Kathryn Parker, RD, LD/N.
2. Increase Brain Metabolism through the Heart, Muscles, and Mind
Research links moderate exercise to increased brain metabolism and improved overall cognition. Exercise need not be too strenuous, but getting the heart rate up, building muscle, and pumping oxygen through your lungs and blood is very beneficial to your mental health. Physical activity can also improve heart conditions (one of the sources of cognitive decline).
Great examples of moderate physical activity include:
- Jogging or brisk walking, especially up an incline or in the sand
- Stretching morning and night
- Gardening and other household tasks
- Cycling either on a stationary bike or along a path
- Tai chi and yoga
- Playing outside with your children or grandchildren
If you’re an athlete who wants to up your game, Aviv will help you achieve your physical goals. Watch the stories of success.

3. Don’t Let Stress Induce Deleterious Effects
If not managed, chronic stress often impairs memory retrieval and information acquisition, even inducing deleterious effects on brain structure and cognition. To help you bounce back from a stressful situation, consider:
- Engaging in physical activity
- Writing your thoughts in a journal
- Getting more sleep—it’s in the downtime that the brain flushes toxins out and cleans itself, allowing the repair you need from spikes of stress
- Doing relaxation techniques such as meditation or breathing exercises
4. Actively Build Neural Pathways
Identify hobbies or activities that keep your mind engaged. For example, one study discovered older adults who took up new body-connected activities that worked the brain in new ways experienced more memory improvement than those who did not.
Here are a few ideas when wondering how to improve your cognitive skills:
- Learn a new language and travel to where you can use it.
- Begin quilting or other detail-oriented crafts.
- Study photography, take pictures, edit them, and share.
- Try reflective therapy, like journaling, to revisit past negative memories and rewrite them more positively (“what I’ve learned” or “how it made me grow”).
- Invest (especially mentally and physically) into your child’s or grandchild’s hobby. Do they play lacrosse? Learn the rules of play and volunteer for the team. Do they have a knack for mathematics? Be their study buddy.
5. Stay in Touch with Your Trusted Physician
It’s essential to discuss cognitive decline with a trusted physician. The more you understand how your health can affect your brain function, the more you can do to safeguard your cognitive vitality. Discuss your options and advocate for yourself to get next-level care that will keep you healthier for the long term.
Fight Cognitive Decline with Aviv

Maintaining your overall health is beneficial for the longevity of your life. Fight cognitive decline with the Aviv Medical Program. Every person’s body and health are unique, and your medical treatment program should reflect that.
Aviv is the leader in brain performance—our program will keep your brain at its best. Our diverse team of medical professionals will provide the customized attention you need to maintain optimal cognitive health and reverse cognitive decline.
Contact us to learn how we can help.
